LGBTQ+ Bulimia Recovery Support Finder
Find Your Path to Recovery
This tool helps you explore treatment options tailored for LGBTQ+ individuals with bulimia nervosa. Answer the questions below to get personalized recommendations.
Recommended Support Options
When talking about eating disorders, Bulimia Nervosa is a pattern of binge eating followed by compensatory actions such as self‑induced vomiting, laxative abuse, or excessive exercise. While it can affect anyone, research shows that queer individuals face extra layers of pressure that can make the disorder harder to recognize and treat.
Key Takeaways
- LGBTQ+ people experience higher rates of bulimia due to minority stress and body‑image ideals.
- Standard treatment works better when providers use LGBTQ+‑affirmative approaches.
- Specialized support options include queer‑focused therapy groups, telehealth, and community helplines.
- Self‑care tools like mindfulness and body‑positive social media can complement clinical care.
- Knowing where to find inclusive providers can shorten the path to recovery.
What Is Bulimia Nervosa?
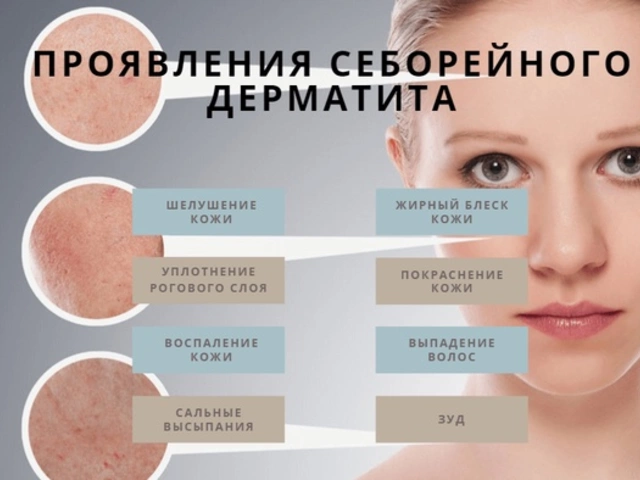
Bulimia Nervosa involves recurring episodes of eating large amounts of food in a short period, followed by behaviors designed to prevent weight gain. Physical signs may include swollen salivary glands, enamel erosion, or frequent sore throats. Psychologically, sufferers often feel intense guilt, shame, and a loss of control around food.
Why the LGBTQ+ Community Is Disproportionately Affected
The LGBTQ+ Community faces unique stressors that intersect with eating‑disorder risk. Minority stress theory explains how stigma, discrimination, and internalised homophobia or transphobia elevate anxiety and body‑image concerns. A 2023 Australian health survey found that 23% of queer youth reported binge‑eating behaviors, compared with 9% of straight peers.
Gender dysphoria can also play a role. Trans and non‑binary individuals may use disordered eating as a way to suppress secondary sex characteristics they find distressing, leading to a higher prevalence of bulimia symptoms.
Social media compounds the issue. Platforms that celebrate hyper‑thin or hyper‑muscular ideals often overlook queer bodies, leaving LGBTQ+ users searching for validation in harmful spaces.

Unique Challenges in Diagnosis and Treatment
- Misdiagnosis: Clinicians may attribute binge‑eating episodes to anxiety or depression without probing eating‑disorder symptoms, especially if the patient does not fit stereotypical “female” profiles.
- Lack of LGBTQ+‑Competent Care: Many therapists have limited training on how gender identity and sexual orientation influence eating‑disorder pathology.
- Stigma Within Communities: Some queer spaces still label eating disorders as a “white, straight‑female” issue, discouraging members from seeking help.
- Family Acceptance: For many young adults, unsupportive families hinder access to care and intensify feelings of isolation.
Support Options That Really Work
| Support Type | Core Focus | Typical Duration | LGBTQ+ Sensitivity | Access |
|---|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Identify and restructure disordered thoughts about food and body. | 12‑20 weekly sessions | Can be LGBTQ+‑affirmative when therapist is trained. | In‑person or telehealth. |
| LGBTQ+ Support Group | Peer sharing, community validation, coping strategies. | Ongoing, weekly or bi‑weekly. | Specifically designed for queer participants. | Community centres, online platforms. |
| Medical Monitoring & Nutritional Counseling | Health check‑ups, electrolyte balance, meal planning. | Monthly check‑ins. | Requires provider aware of hormone therapy interactions. | Specialist clinics or tele‑nutrition services. |
| SSRIs (e.g., Fluoxetine) | Reduce binge‑urge frequency and anxiety. | Prescribed long‑term, reviewed quarterly. | Prescriber must consider interaction with gender‑affirming meds. | Psychiatrist or GP. |
| Online Tele‑Therapy Platforms | Flexible, private counseling sessions. | Variable, based on client need. | Many platforms now list LGBTQ+‑affirmative clinicians. | Internet‑based, often covered by insurance. |
Choosing the right mix depends on personal comfort, location, and whether you’re also navigating hormone therapy or transition‑related care. For many, a combination of CBT and a queer‑focused support group provides both professional guidance and community affirmation.
How to Find LGBTQ+‑Affirmative Care
- Search LGBTQ+ provider directories such as Healthline’s “Queer Therapist Finder” or the Australian “Psychology Australia LGBTQ+ List”.
- Ask your primary doctor for referrals to clinicians who have documented training in gender‑affirming care.
- Check therapist bios for phrases like “affirmative”, “minority stress‑informed”, or “experience with eating disorders in queer populations”.
- Read client reviews that mention respect for pronouns and cultural competence.
- Schedule a brief introductory call to gauge comfort level before committing to a full treatment plan.
Even if a provider isn’t explicitly queer‑focused, you have the right to request an inclusive approach. Many therapists are willing to adapt once they understand your needs.
Self‑Help Strategies to Complement Professional Care
- Mindful Eating: Slow down meals, notice hunger cues, and practice gratitude for the food you’re consuming.
- Body‑Positive Media: Follow LGBTQ+ creators who celebrate diverse bodies and challenge dieting culture.
- Journaling: Write about triggers, emotions, and successes; this helps track patterns and reinforces progress.
- Breathing & Grounding Exercises: Use 4‑7‑8 breathing or 5‑4‑3‑2‑1 grounding to curb binge urges.
- Peer Support Apps: Safe, moderated forums like “Rethink Health” or “7 Cups” host queer‑friendly spaces.
These tactics are not a substitute for therapy, but they can reduce the frequency of binge‑purge cycles and boost self‑esteem between appointments.
Resources & Crisis Helplines
- Lifeline Australia (131114) - 24/7 mental‑health crisis line, LGBTQ+‑aware staff.
- Kids Helpline (1800551800) - Confidential support for ages 5‑25, includes eating‑disorder help.
- Trans Lifeline (877‑565‑8860) - Peer‑run, specialises in trans‑specific mental‑health crises.
- Elephant Talk (1800555111) - Australian service focusing on eating‑disorder recovery, LGBTQ+‑friendly.
- EatRightNow (online chat) - Free chat with registered dietitians trained in queer health.
Never wait for a perfect moment to call; reaching out early can prevent complications like electrolyte imbalance or severe depression.
Frequently Asked Questions
Can bulimia nervosa be cured?
Recovery is possible for most people, but it often involves ongoing management. A blend of therapy, medical monitoring, and supportive community reduces relapse risk.
Why does my therapist need to know I’m LGBTQ+?
Your identity shapes body image, coping mechanisms, and experiences of discrimination. An affirming therapist can tailor interventions to address these specific stressors.
Are there medication options that work with hormone therapy?
Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine are commonly prescribed for bulimia and generally do not interfere with estrogen or testosterone regimens. Always discuss dosage with a psychiatrist familiar with gender‑affirming care.
How can I find a queer‑focused support group online?
Websites such as Meetup, TikTok, and the National Eating Disorders Association list LGBTQ+‑specific groups. Look for clear moderator guidelines and a statement of confidentiality.
What signs tell me I need urgent medical help?
Severe dehydration, fainting, persistent vomiting, sudden weight loss, or suicidal thoughts require immediate attention-call emergency services (000 in Australia) or go to the nearest hospital.
Understanding the intersection of bulimia nervosa and queer identity is the first step toward getting the right help. With knowledgeable clinicians, supportive peers, and practical self‑care tools, recovery is within reach.






Comments(13)