Leukeran vs. Other Cancer Drugs Comparison Tool
Recommended Drug Based on Your Profile:
Why This Choice?
Drug Comparison Table
| Drug | Mechanism | Route | Typical Dose | Side Effects | Average Monthly Cost (US$) |
|---|---|---|---|---|---|
| Leukeran (Chlorambucil) | Alkylating agent - DNA cross-linking | Oral | 0.1-0.5 mg/kg daily | Nausea, fatigue, myelosuppression | ≈ $150 |
| Bendamustine | Alkylating + antimetabolite | IV (days 1-2) | 70 mg/m² | Neutropenia, infusion reactions | ≈ $3,200 |
| Fludarabine | Purine analogue - DNA synthesis inhibition | IV (days 1-3) | 25 mg/m² | Lymphopenia, infections, neurotoxicity | ≈ $2,800 |
| Ibrutinib | BTK inhibitor - B-cell receptor signaling blockade | Oral | 420 mg daily | Atrial fibrillation, bleeding, diarrhea | ≈ $9,500 |
| Venetoclax | BCL-2 inhibitor - promotes apoptosis | Oral | Ramp to 400 mg daily | Tumor-lysis syndrome, neutropenia | ≈ $12,000 |
| Rituximab | Anti-CD20 monoclonal antibody | IV | 375 mg/m² weekly ×4 | Infusion reactions, hepatitis B reactivation | ≈ $4,500 |
When a doctor writes a prescription for Leukeran (chlorambucil), patients often wonder if there’s a better fit for their type of leukemia or lymphoma. The answer isn’t one‑size‑fits‑all; it depends on disease stage, other health issues, and how the drug’s side‑effect profile matches a person’s lifestyle. This guide breaks down Leukeran, shows where it shines, and measures it against the most common alternatives used today.
Key Takeaways
- Leukeran is an oral alkylating agent that is affordable and easy to take, but it works slower than newer targeted drugs.
- For early‑stage chronic lymphocytic leukemia (CLL) in patients without high‑risk genetic markers, Leukeran remains a solid first‑line choice.
- Targeted therapies such as ibrutinib or venetoclax give deeper, faster remissions but carry higher price tags and distinct toxicities.
- Combination regimens (e.g., bendamustine+rituximab) can boost response rates but require IV visits and close monitoring.
- Choosing the right drug involves balancing efficacy, side‑effects, cost, and convenience - the checklist at the end helps you weigh each factor.
What Is Leukeran (Chlorambucil)?
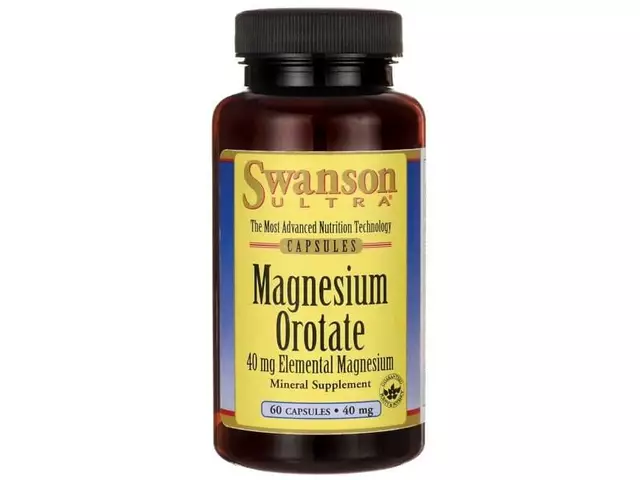
Leukeran is the brand name for chlorambucil, an oral alkylating chemotherapy first approved by the FDA in 1958. It belongs to the class of nitrogen‑mustard agents that add alkyl groups to DNA, disrupting cancer cell replication. Typical dosing for CLL is 0.5 mg/kg daily for 14 days every 28‑day cycle, though many clinicians use a lower, continuous daily dose (0.1 mg/kg) for older patients.
How Leukeran Works
Chlorambucil’s mechanism is straightforward: it forms covalent bonds with the guanine bases of DNA, causing cross‑links that prevent the double‑helix from separating during cell division. This damage triggers apoptosis in rapidly dividing B‑cells, the culprits behind CLL and some low‑grade non‑Hodgkin lymphomas. Because the drug targets DNA directly, it’s not selective for cancer cells, which explains its broader side‑effect spectrum.
Common Alternatives to Leukeran
Below are the most frequently prescribed drugs that either replace or complement chlorambucil in modern regimens.
- Bendamustine is a bifunctional alkylating agent approved in 2008 for CLL and indolent NHL. It is given intravenously (IV) on days 1 and 2 of a 28‑day cycle.
- Fludarabine is a purine analogue that interferes with DNA synthesis, usually administered IV on days 1-3 of a 28‑day cycle.
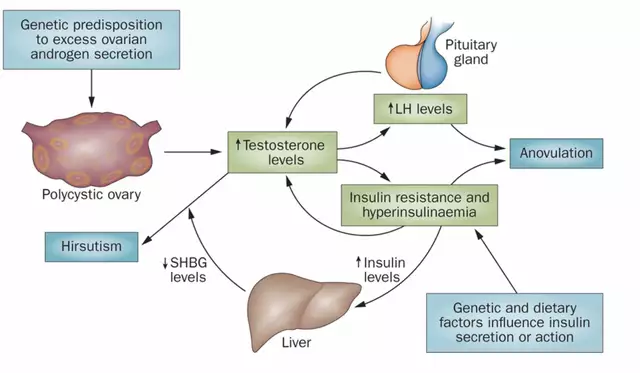
- Ibrutinib is a first‑in‑class Bruton’s tyrosine kinase (BTK) inhibitor taken orally once daily, revolutionizing CLL treatment since its 2014 approval.
- Venetoclax is a BCL‑2 inhibitor that induces rapid apoptosis, taken orally with a weekly dose‑ramp schedule.
- Rituximab is a monoclonal antibody against CD20‑positive B‑cells, given IV weekly for four weeks in most CLL protocols.
- Obinutuzumab is a glycoengineered anti‑CD20 antibody with higher affinity, administered IV on a schedule similar to rituximab.
Side‑Effect Profiles
Understanding toxicity is key when swapping drugs.
- Leukeran: nausea, fatigue, myelosuppression (low blood counts), and rare secondary cancers.
- Bendamustine: stronger neutropenia, infusion‑related reactions, and higher risk of infections.
- Fludarabine: profound lymphopenia, opportunistic infections, and neurologic toxicity at high doses.
- Ibrutinib: atrial fibrillation, hypertension, bleeding, and diarrhea.
- Venetoclax: tumor‑lysis syndrome (especially in high‑burden disease), neutropenia, and gastrointestinal upset.
- Rituximab/Obinutuzumab: infusion reactions, hepatitis B reactivation, and modest cytopenias.
Side‑Effect Comparison Table
| Drug | Mechanism | Route | Typical Dose | FDA Approval Year | Common Side Effects | Average Monthly Cost (US$) |
|---|---|---|---|---|---|---|
| Leukeran (Chlorambucil) | Alkylating agent - DNA cross‑linking | Oral | 0.1-0.5mg/kg daily | 1958 | Nausea, fatigue, myelosuppression | ≈$150 |
| Bendamustine | Alkylating + antimetabolite | IV (days1‑2) | 70mg/m² | 2008 | Neutropenia, infusion reactions | ≈$3,200 |
| Fludarabine | Purine analogue - DNA synthesis inhibition | IV (days1‑3) | 25mg/m² | 1991 | Lymphopenia, infections, neurotoxicity | ≈$2,800 |
| Ibrutinib | BTK inhibitor - B‑cell receptor signaling blockade | Oral | 420mg daily | 2014 | Atrial fibrillation, bleeding, diarrhea | ≈$9,500 |
| Venetoclax | BCL‑2 inhibitor - promotes apoptosis | Oral | Ramp to 400mg daily | 2016 | Tumor‑lysis syndrome, neutropenia | ≈$12,000 |
| Rituximab | Anti‑CD20 monoclonal antibody | IV | 375mg/m² weekly ×4 | 1997 | Infusion reactions, hepatitis B reactivation | ≈$4,500 |
When Leukeran Still Makes Sense
Even with high‑tech drugs on the market, Leukeran remains a go‑to for several scenarios:
- Older patients (≥75years) with limited comorbidities: The oral route avoids frequent clinic trips, and low‑dose regimens are well tolerated.
- Low‑risk CLL (no TP53 deletion, IGHV‑mutated): Studies show similar overall survival between chlorambucil and newer agents when used as first‑line monotherapy.
- Cost‑sensitive settings: Generic chlorambucil is dramatically cheaper than targeted oral agents, making it attractive for uninsured or under‑insured patients.
- Combination strategies: In many clinical trials, chlorambucil paired with anti‑CD20 antibodies (e.g., obinutuzumab) yields response rates close to ibrutinib, but at a fraction of the cost.
Decision Checklist - Is Leukeran Right for You?
- Do you prefer an oral pill over IV infusions? → Leukeran scores high.
- Is your disease genetically low‑risk? → Yes → Leukeran remains effective.
- Do you have a history of heart rhythm problems? → Consider avoiding ibrutinib.
- Is budget a major concern? → Chlorambucil is the most affordable option.
- Do you need rapid disease control (e.g., high tumor burden)? → Targeted agents or combination chemo‑immunotherapy may act faster.
How to Transition Between Therapies
Switching from Leukeran to a newer drug (or vice‑versa) should be done under close supervision:
- Confirm complete blood count has recovered to safe levels (ANC>1.5×10⁹/L, platelets>100×10⁹/L).
- Stop chlorambucil at least 48hours before starting an IV agent to minimize overlapping myelosuppression.
- If moving to ibrutinib or venetoclax, perform a wash‑out period of 5‑7days; monitor ECG for ibrutinib‑related arrhythmias.
- Educate the patient on new drug-specific toxicities (e.g., tumor‑lysis for venetoclax) and arrange labs on day1,3,7, and weekly thereafter.
Future Trends
Research is pushing chlorambucil into combination regimens with novel agents. Ongoing PhaseIII trials pair low‑dose chlorambucil with the BTK inhibitor zanubrutinib, aiming for a cost‑effective yet deep response. If these studies succeed, the line between “old‑school chemo” and “targeted therapy” may blur, giving patients more personalized options.
Frequently Asked Questions
Can I take Leukeran and ibrutinib together?
Concurrent use is not standard because both suppress bone marrow and increase infection risk. If a physician decides to combine them for a specific protocol, they will schedule staggered dosing and monitor blood counts weekly.
How long does a typical Leukeran course last?
Most clinicians prescribe continuous daily dosing until disease progression or unacceptable toxicity. Some use a 14‑day on/14‑day off schedule, repeating every 28days, especially in older patients.
Is Chlorambucil suitable for patients with kidney problems?
Yes, chlorambucil is largely excreted unchanged in the urine, but dosage reductions are recommended when creatinine clearance falls below 30mL/min to avoid excess toxicity.
What monitoring is needed while on Leukeran?
Baseline CBC, liver function, and renal labs are required. After starting therapy, CBC should be checked every 2‑4weeks for the first two cycles, then monthly if stable.
Are there any dietary restrictions with Chlorambucil?
No strict restrictions, but staying hydrated helps kidney clearance. Alcohol should be limited, as both can worsen liver toxicity.
Next Steps
Talk to your oncologist about where you fall on the risk spectrum, your budget, and how much time you can spend on clinic visits. Bring this comparison sheet to the appointment - it makes the conversation concrete and helps the doctor explain why a particular drug is suggested. If you’re looking for a cheaper option, ask specifically about generic chlorambucil and whether a combination with an anti‑CD20 antibody is covered by your insurance.




Comments(16)