Imagine waking up and immediately thinking, What if I accidentally hit someone with my car? Or maybe you wash your hands until they bleed because you touched a doorknob. You know it doesn’t make sense. You’re not a dangerous person. You’re not dirty. But the thought won’t leave. And if you don’t do the ritual - the checking, the counting, the silent praying - the anxiety crashes over you like a wave. This isn’t just being neat or cautious. This is OCD.
What Are Intrusive Thoughts in OCD?
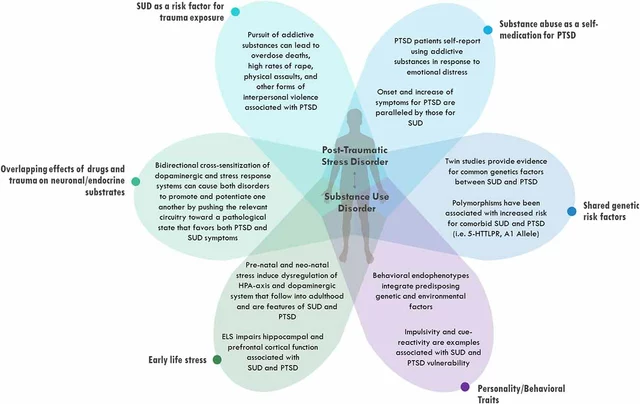
Intrusive thoughts aren’t unique to OCD. Everyone has them. Maybe you’ve had a fleeting image of yelling at your boss or pushing someone in front of a train. Most people brush them off: That was weird, but it’s just a thought. People with OCD don’t get that luxury. In OCD, these thoughts stick. They feel dangerous. They feel like signs. A parent might think, What if I drop my baby? - and then spend hours mentally replaying every time they held the child, convinced they almost did it. Someone else might obsess over whether they offended a coworker with a glance, replaying the conversation 50 times. These aren’t desires. They’re not intentions. They’re terrifying, unwanted, and feel completely out of character. Research shows that about 20-25% of people with OCD have harm-related obsessions. Another 25% struggle with contamination fears. Around 10-15% are haunted by taboo thoughts - sexual, religious, or identity-based - that make them feel ashamed and isolated. One Reddit user wrote: I’ve never hurt anyone. But I have violent images 10 times a day. I feel like a monster. That’s the heart of it. The thoughts feel alien. They conflict with everything the person believes about themselves. That’s called ego-dystonic. The brain doesn’t treat these thoughts like random noise. In people with OCD, the orbitofrontal cortex and caudate nucleus - areas tied to fear and decision-making - go into overdrive. fMRI scans show these regions light up like Christmas trees when someone with OCD is triggered. The brain screams, Danger! - even when there’s no real threat.Why Compulsions Make It Worse
When the thought hits, the anxiety spikes. And the mind scrambles for relief. That’s when compulsions kick in. Handwashing. Checking the stove. Repeating a phrase in your head. Avoiding certain numbers. Counting steps. Praying silently. These aren’t habits. They’re survival tactics. They feel like the only thing stopping something terrible from happening. But here’s the trap: every time you do the compulsion, you’re teaching your brain that the thought was dangerous - and that you needed the ritual to stay safe. It’s a loop:- Obsession: A thought pops in - What if I’m gay and I don’t know it?
- Anxiety: Panic. Shame. Dread. Your heart races.
- Compulsion: You mentally review past relationships. You check your reactions to people. You Google symptoms.
- Temporary relief: The panic fades… for a few minutes.
- Back to step one: The thought returns - louder this time.
ERP Therapy: The Only Proven Way Out
There’s one treatment that consistently works: Exposure and Response Prevention, or ERP. It’s not talk therapy. It’s not mindfulness. It’s not medication alone. ERP is the gold standard - backed by decades of research and endorsed by the American Psychological Association. ERP works by breaking the loop. No more rituals. No more avoidance. Instead, you face the thought - on purpose - and let the anxiety rise without doing anything to make it go away. Let’s say you’re terrified of contaminating your family with germs. Your ERP therapist might ask you to:- Touch a bathroom doorknob (anxiety level: 30/100)
- Then eat a snack without washing your hands (anxiety level: 75/100)
- Then sit on a public bench and touch your face (anxiety level: 90/100)

What ERP Doesn’t Look Like
ERP isn’t about being tough. It’s not about “just facing your fears.” It’s not about pushing through panic like a soldier. It’s structured. It’s slow. It’s guided. You don’t start with the worst fear. You start with something that feels 30% scary. You build a ladder. One rung at a time. And you do it repeatedly - often for 12 to 20 weeks. And yes, it’s hard. About 70% of people feel worse in the first two weeks. The anxiety spikes. You want to quit. That’s normal. That’s the brain fighting back. Dropout rates are high - about 25% - because it’s uncomfortable. But the people who stick with it? They get their lives back. A 14-year-old in a CDC case study went from spending 4-5 hours a day in compulsions to less than 30 minutes after six months of ERP. She went from hiding in her room to going to school, hanging out with friends, sleeping through the night.Medication and ERP: Do You Need Both?
Medication - usually SSRIs like fluoxetine or sertraline - can help reduce the intensity of obsessions. But it doesn’t teach your brain to stop reacting. It just turns down the volume. ERP teaches your brain to stop listening. Combining ERP with medication works best for many people - up to 85% respond. But 30% of those on medication stop because of side effects: nausea, weight gain, low sex drive, emotional numbness. If you’re on meds and still stuck in the cycle? ERP is what you need. If you’re not on meds and your symptoms are severe? Talk to a doctor. But don’t wait for meds to “fix” you before starting ERP. ERP is the treatment. Medication is a helper.Why Most Therapists Can’t Help
Here’s the cruel part: most therapists don’t know how to do ERP. General CBT? It often makes OCD worse. Talking about your thoughts? That’s rumination. Reassuring yourself? That’s a compulsion. Saying, “It’s just a thought, it doesn’t mean anything”? That’s not ERP. That’s reinforcing the idea that the thought is dangerous - and needs to be reasoned with. Only about 10% of U.S. therapists are trained in evidence-based OCD treatment. In rural areas, that number drops to zero. Many people wait over 10 years to get the right diagnosis. Telehealth has helped. Now 45% of people get ERP online. But insurance often won’t cover it equally. You might pay $200 an hour for a specialist - or pay nothing for someone who doesn’t know what they’re doing.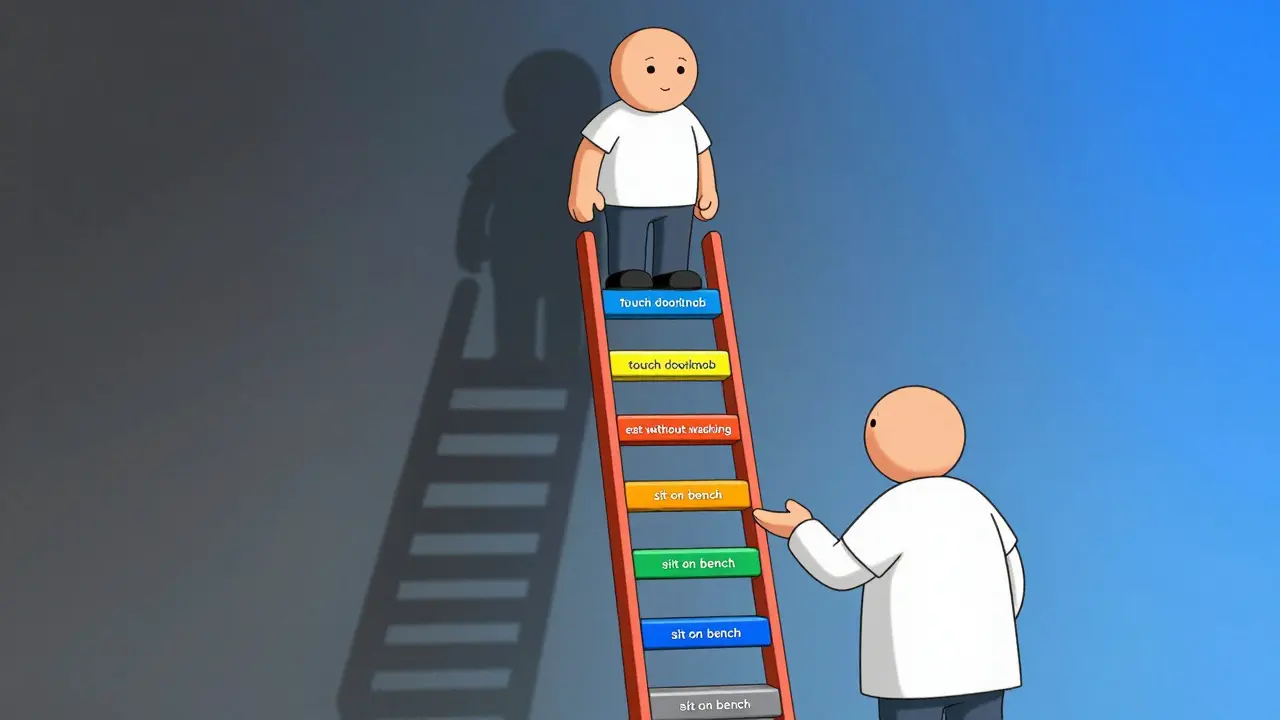
New Tools, Same Goal
The FDA approved the first digital therapeutic for OCD in 2023: the nOCD app. It guides users through ERP exercises, tracks progress, and connects them to certified therapists. In a 2022 study, it helped 55% of people with mild OCD reduce symptoms. Stanford researchers are using AI to predict who will respond to ERP - using brain scans to spot patterns before treatment even starts. Transcranial magnetic stimulation (TMS) is showing promise for those who don’t respond to ERP or meds - 45% improvement in a 2023 study. But none of these replace ERP. They just make it more accessible.You’re Not Broken
You didn’t choose this. You didn’t cause this. Your thoughts don’t define you. The fact that you’re horrified by them? That’s proof you’re not the person your OCD says you are. You’re not a monster. You’re not weak. You’re someone whose brain got stuck in a loop - and you’re ready to break it. ERP isn’t about becoming fearless. It’s about learning to live with uncertainty. About trusting that you can feel anxious and still be safe. About realizing that you don’t need to control your thoughts to be okay. It takes work. It takes time. But it’s the only path that leads out of the cage.Where to Start
If you think you have OCD:- Find a therapist trained in ERP. Use the IOCDF’s therapist directory.
- Don’t wait for meds to “fix” you before starting therapy.
- Join a support group. You’re not alone. Over 125,000 people on Reddit’s r/OCD know exactly what you’re going through.
- Be patient. The first few weeks are the hardest. But they’re the most important.





Comments(12)