Medication Safety Assessment Tool
Medication Safety Assessment
This tool helps assess potential medication risks for post-menopausal women. Based on your inputs, we'll identify medications that may need review with your healthcare provider.
When a woman hits menopause, her body changes in ways that go far beyond hot flashes and sleepless nights. Hormones shift, metabolism slows, and how her body handles medications changes too. Yet many doctors still treat post-menopausal women the same way they treat younger patients - and that’s where things can go wrong. Medication safety isn’t just about taking pills correctly; it’s about knowing which drugs are safe, which ones are risky, and when to stop them entirely.
Why Medications Act Differently After Menopause
After menopause, estrogen levels drop sharply. That doesn’t just affect mood or bone density - it changes how your liver and kidneys process drugs. Oral estrogen, for example, goes straight to the liver on its first pass, increasing the risk of blood clots. Transdermal patches, on the other hand, bypass the liver and cut that risk by 30-50%. That’s not a small difference. It’s the difference between staying out of the hospital and ending up in one. Many women in their 60s and 70s take four or five prescriptions daily. Some take even more. The National Poll on Healthy Aging found that 56% of Americans over 65 are women, and they’re more likely than men to be on multiple medications. That’s not because they’re sicker - it’s because they live longer, and chronic conditions pile up. High blood pressure. Arthritis. Diabetes. High cholesterol. Each condition brings its own drug. And when you’re on five or more, the chance of a bad reaction jumps dramatically.What Not to Take: Absolute and Conditional Red Flags
The Endocrine Society laid out clear rules in 2015: estrogen therapy is absolutely off-limits if you’ve had breast cancer, a history of blood clots, liver disease, or unexplained vaginal bleeding. These aren’t suggestions. They’re hard stops. Yet, some providers still prescribe hormone therapy to women with these conditions - often because they’re trying to relieve symptoms without fully understanding the risks. Even if you don’t have those absolute contraindications, some conditions require caution. If you have high triglycerides (over 400 mg/dL), oral estrogen can push them even higher, raising your risk of pancreatitis. If you have diabetes, estrogen can make blood sugar harder to control. Migraines with aura? Oral estrogen can triple your stroke risk. The American Heart Association says to avoid it entirely. And then there’s the issue of progestins. Combined estrogen-progestin therapy increases breast cancer risk by 24% after five years, according to the Women’s Health Initiative. That’s why the U.S. Preventive Services Task Force recommends against using it for chronic disease prevention. If you’ve had a hysterectomy, estrogen alone may be safer - but only if started early, before age 60.Hormone Therapy Alternatives: What Actually Works
Not every woman needs hormones. And not every woman should take them. For hot flashes, non-hormonal options like SSRIs (such as paroxetine) can reduce symptoms by 50-60%. But here’s the catch: 30-40% of women on these drugs report sexual side effects - lower desire, trouble with arousal. That’s a trade-off many aren’t told about. Tibolone, used in Europe but not approved in the U.S., cuts fracture risk by nearly half. But it also increases stroke risk by 58%. That’s not a win. It’s a gamble. Newer options like conjugated estrogens/bazedoxifene (a tissue-selective estrogen complex) offer a better balance. In the SMART-5 trial, this combo reduced endometrial thickening by 70% compared to traditional hormone therapy - meaning less risk of uterine cancer without needing a progestin. It’s not perfect, but for some women, it’s the best middle ground.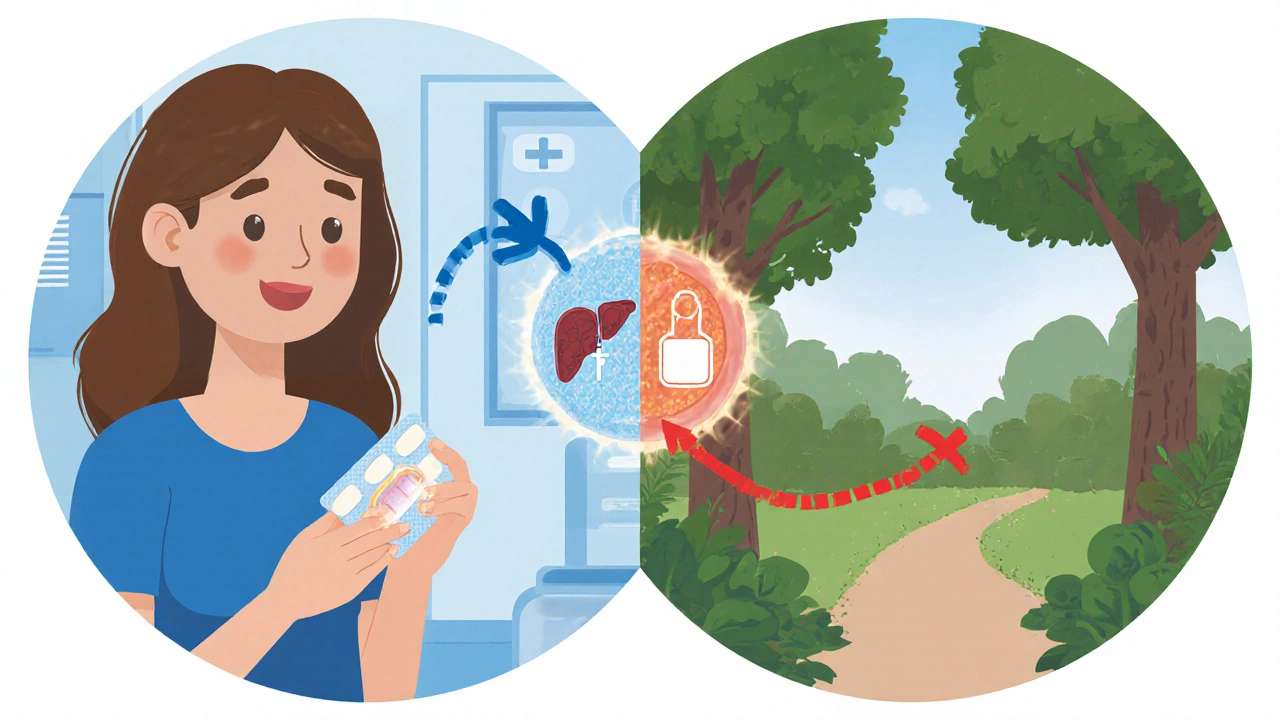
Polypharmacy: When More Medicines Mean More Danger
Polypharmacy isn’t just a buzzword. It’s a silent killer. The World Health Organization calls it a global priority. Four out of ten older adults get prescriptions from different doctors - no one is putting all the pieces together. A woman might see her cardiologist for blood pressure, her rheumatologist for arthritis, her gynecologist for hot flashes, and her primary care doctor for cholesterol. Each one writes a script. No one asks: Are these safe together? The results? A 72-year-old woman in a WHO case study was on diclofenac (an NSAID), simvastatin, enalapril, and atenolol. She kept taking the diclofenac even after being told to stop. Within a week, her hemoglobin dropped from 12.5 to 8.1 g/dL. She ended up hospitalized with a bleeding ulcer. That’s not rare. That’s typical. The Beers Criteria lists 30 medications that should be avoided in older adults. Long-acting benzodiazepines? They increase hip fracture risk by 50%. Anticholinergics like diphenhydramine (Benadryl)? They raise dementia risk. These drugs are still prescribed - often because the doctor doesn’t know better, or the patient doesn’t speak up.Deprescribing: The Art of Stopping
Stopping medication is just as important as starting it. Yet most doctors aren’t trained to do it. Deprescribing isn’t about cutting corners - it’s about removing what’s no longer needed. The WHO found that structured deprescribing reduces medication burden by 1.4 drugs per person and cuts adverse events by 33%. But it takes time. You can’t just quit a beta-blocker or an antidepressant cold turkey. Benzodiazepines need 8-12 weeks to taper safely. Antidepressants need 4-8 weeks. Each reduction should be slow, monitored, and documented. And it should be a conversation - not a decision made in 5 minutes during a busy appointment. The START/STOPP criteria help. It’s a tool that identifies 116 inappropriate medications and 81 underused ones in older adults. If your doctor doesn’t use it, ask them why.
How to Take Control of Your Medications
You don’t have to wait for your doctor to fix this. Here’s what you can do today:- Keep a current list of every pill, supplement, and herb you take - including doses and why you take them.
- Bring all your medications to every appointment - in a bag, not a list. This is called a “brown bag review.”
- Use a pill organizer. Studies show they reduce errors by 81%. But don’t just fill it once and forget it. Check it weekly.
- Ask: “Is this still necessary?” every time a new prescription comes in.
- Ask: “What happens if I stop this?” before starting anything new.
- Get a medication therapy review if you’re on Medicare Part D - it’s free, and it’s required annually if you have multiple chronic conditions.
The Real Cost of Getting It Wrong
Bad medication management isn’t just risky - it’s expensive. In the U.S., medication errors in older adults cost $26 billion a year. One in three hospitalizations for women over 65 is caused by a drug reaction. And half of all chronic disease meds are prescribed, dispensed, or taken incorrectly. The good news? You’re not powerless. The FDA now requires menopausal safety info on 87% of relevant drug labels. Research into tissue-selective therapies and pharmacogenomics (testing how your genes affect drug response) is moving fast. AI tools are being tested to flag dangerous interactions before they happen. But none of that matters if you don’t ask the right questions. If your doctor doesn’t talk about deprescribing, bring it up. If you’re on five or more meds and no one’s reviewed them in a year, schedule a dedicated appointment. Your life depends on it.Is hormone therapy safe for post-menopausal women?
Hormone therapy can be safe for some women, but only if started early (before age 60 or within 10 years of menopause) and tailored to individual risk. Transdermal estrogen is safer than oral for women with clotting risks. Estrogen alone may be an option for those without a uterus. Combined estrogen-progestin is not recommended for chronic disease prevention due to increased breast cancer, stroke, and blood clot risks. Always weigh symptom relief against long-term safety.
What are the biggest medication risks for post-menopausal women?
The biggest risks come from polypharmacy - taking too many drugs at once. NSAIDs like ibuprofen and diclofenac can cause dangerous bleeding, especially in older women. Long-acting benzodiazepines increase fall and fracture risk by 50%. Anticholinergics (like Benadryl) are linked to higher dementia risk. Oral estrogen raises blood clot risk, and combined hormone therapy increases breast cancer risk. Many of these are still prescribed without proper review.
Can I stop my medications on my own if I feel better?
No. Stopping certain medications suddenly can be dangerous. Blood pressure drugs, antidepressants, and beta-blockers can cause rebound effects - spikes in blood pressure, panic attacks, or heart rhythm problems. Always talk to your doctor before stopping. If you want to reduce your meds, ask about a structured deprescribing plan with gradual tapering.
What’s the difference between transdermal and oral hormone therapy?
Oral estrogen passes through the liver first, which increases clotting factors and liver strain. Transdermal estrogen (patches, gels) enters the bloodstream directly, avoiding the liver. This reduces the risk of blood clots by 30-50%. It’s also more stable in the body, with fewer spikes and dips in hormone levels. For women with a history of clots, migraines with aura, or high triglycerides, transdermal is the preferred option.
How often should I get a medication review?
At least once a year - and more often if you’ve been hospitalized, started or stopped two or more medications, or if you’re over 65 and taking five or more drugs. Medicare Part D beneficiaries with multiple chronic conditions are entitled to a free annual medication therapy review. Bring all your pills in a bag - not just a list - so your pharmacist or doctor can see everything you’re taking.
Are natural remedies safer than prescription drugs for menopause symptoms?
Not necessarily. Many herbal supplements like black cohosh, red clover, or soy isoflavones aren’t regulated like prescription drugs. They can interact with blood thinners, thyroid meds, or antidepressants. Some contain hidden estrogen-like compounds that could be risky if you have a history of breast cancer. Always tell your doctor what you’re taking - even if you call it “natural.”





Comments(9)