Tizanidine-Ciprofloxacin Interaction Checker
Check Your Medication Risk
This tool identifies if you're taking a dangerous combination of tizanidine (muscle relaxant) and ciprofloxacin (antibiotic). This combination can cause severe low blood pressure and extreme drowsiness.
Two common prescriptions - one for muscle spasms, another for a urinary tract infection - might seem harmless on their own. But when taken together, they can send your blood pressure crashing and leave you too drowsy to stand. This isn’t theoretical. It’s happening in clinics right now, even though doctors and pharmacists have known about it for years.
What Happens When Tizanidine Meets Ciprofloxacin
Tizanidine is a muscle relaxant. It works by calming overactive nerves in your spinal cord, helping with back pain, neck stiffness, or spasticity from conditions like multiple sclerosis. Ciprofloxacin is an antibiotic - a fluoroquinolone - used to treat bacterial infections like pneumonia, kidney infections, or sinusitis. On paper, they do different jobs. But inside your body, they collide. The problem lies in how your liver breaks down tizanidine. About 95% of it is processed by a single enzyme: CYP1A2. Ciprofloxacin doesn’t just touch this enzyme - it shuts it down. Hard. When you take ciprofloxacin, your body can’t clear tizanidine the way it should. Instead of being broken down and flushed out, tizanidine builds up. Studies show levels can spike 10 to 33 times higher than normal. That’s not a small increase. That’s a medical emergency waiting to happen.The Real Risks: Low Blood Pressure and Deep Sedation
High tizanidine levels don’t just make you sleepy - they can knock your blood pressure into dangerous territory. Severe hypotension means your systolic pressure drops below 70 mm Hg. At that point, your brain and organs don’t get enough blood. You might feel dizzy, nauseous, or faint. In worst-case scenarios, you pass out, hit your head, or need emergency IV fluids and medications just to stabilize your pressure. Sedation isn’t mild either. People report being unable to stay awake, slurring speech, or needing hospitalization because they couldn’t wake up. One patient in a WHO pharmacovigilance database reported being found unconscious at home after taking both drugs. He spent three days in the hospital. These aren’t rare outliers. A study from Vanderbilt University Medical Center, analyzing real patient records, found a 43% higher chance of severe low blood pressure when these two drugs were taken together. That’s not a 5% risk. That’s nearly half again more likely to land you in the ER.Why This Interaction Is Unique to Tizanidine
Not all muscle relaxants behave like this. Cyclobenzaprine, another common one, is broken down by multiple liver enzymes. If one pathway gets blocked, others can still clear the drug. Tizanidine doesn’t have that safety net. It relies entirely on CYP1A2. That’s why it’s uniquely vulnerable. This is why experts like Dr. Cecilia Chung and her team at Vanderbilt call this interaction “a perfect storm.” Ciprofloxacin isn’t the only offender - fluvoxamine (an antidepressant), amiodarone (a heart rhythm drug), and even some over-the-counter supplements like St. John’s Wort in certain forms can do the same thing. But ciprofloxacin is one of the most common antibiotics prescribed, especially to older adults with UTIs - the exact group also likely to be on tizanidine for chronic back pain.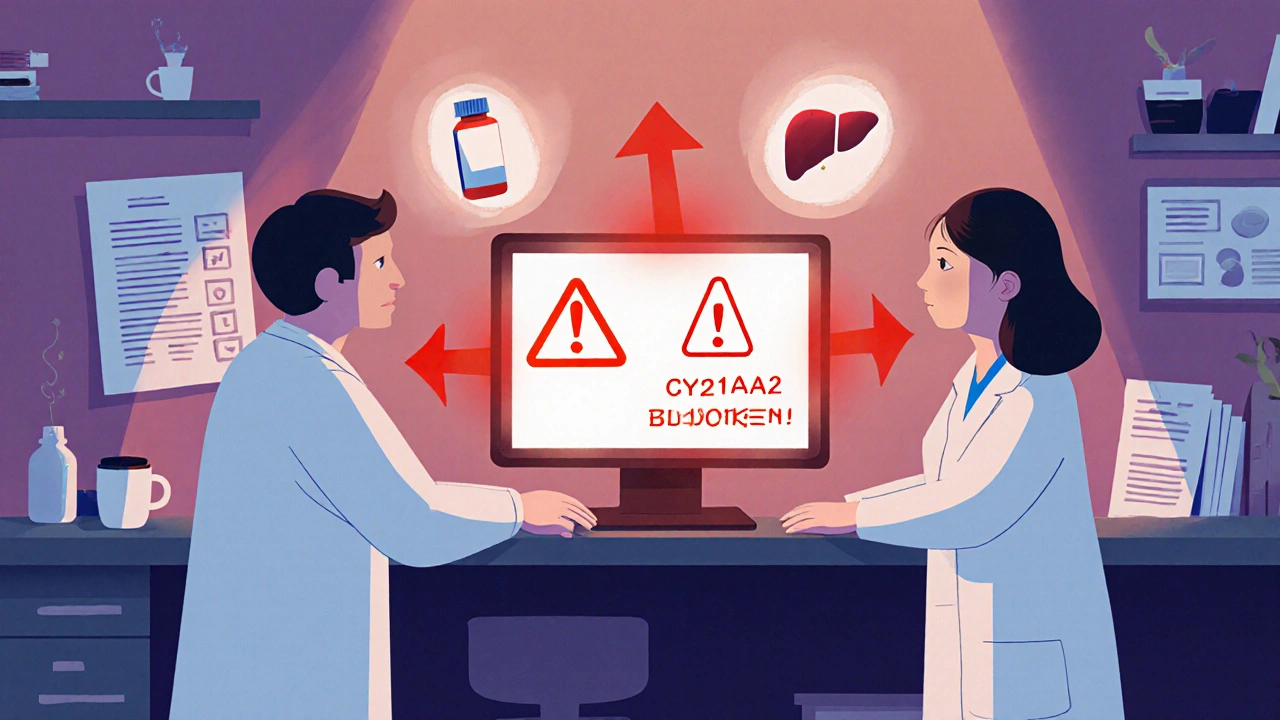
Who’s Most at Risk?
You’re at higher risk if:- You’re over 65
- You’re already taking blood pressure meds (like lisinopril, amlodipine, or hydrochlorothiazide)
- You have kidney or liver problems
- You take more than three other medications
What Doctors Should Do - And What They Often Don’t
The FDA and EMA both list this combination as contraindicated. That means it’s officially unsafe. The tizanidine package insert says it outright: “Do not use with CYP1A2 inhibitors like ciprofloxacin.” Yet, it still happens. Why? Because doctors aren’t always thinking about drug metabolism. A patient comes in with a bad back and a UTI. The doctor prescribes tizanidine for the pain and ciprofloxacin for the infection. They don’t connect the dots. The pharmacist might miss it too - especially if the prescription comes through electronically without a clear alert. A 2019 study found that even with formal warnings, this combo was still being prescribed in routine care. That’s not just negligence - it’s a systemic failure in how we train prescribers and design electronic health systems.What to Do If You’re on Tizanidine and Need an Antibiotic
If you’re taking tizanidine and your doctor says you need an antibiotic, ask this:- Is ciprofloxacin absolutely necessary?
- Are there alternatives that don’t block CYP1A2?
- Amoxicillin (for UTIs, sinus infections)
- Nitrofurantoin (for uncomplicated UTIs)
- Cephalexin (for skin or respiratory infections)

What to Do If You’ve Already Taken Both
If you accidentally took tizanidine and ciprofloxacin together:- Do not drive or operate machinery
- Stay seated or lying down - don’t stand up quickly
- Check your blood pressure if you have a home monitor
- Call your doctor or poison control immediately if you feel faint, dizzy, or unusually sleepy






Comments(15)