When you pick up a prescription, you might assume that if it’s generic, you’re already getting the best deal. But that’s not always true. Some generic drugs cost more than others-even when they do the exact same thing. And in many cases, there’s a cheaper option hiding in plain sight: a different generic version, a different strength, or even a combination pill that replaces two separate drugs. The truth is, generic combination products and smart therapeutic substitutions can save you hundreds, sometimes thousands, of dollars a year-without sacrificing effectiveness.
Why Some Generics Cost More Than Others
Not all generics are created equal. A 2022 study of over 1,000 generic drugs in Colorado found that some generics were priced at 15 times more than other versions of the same medication. For example, one generic version of a common blood pressure pill cost $7.50 per pill, while another, equally effective version, cost just $0.48. That’s a 94% difference. And this wasn’t an outlier. Out of 45 high-cost generics identified in the study, nearly all had cheaper alternatives with the same active ingredients and clinical results. The reason? It’s not about quality. It’s about market competition. When only one or two companies make a generic drug, they can charge more. But when five or six companies enter the market, prices drop fast. The FDA found that with three or more generic manufacturers, prices fall by about 20% within three years-and keep falling as more players join. Some drugs, like Crestor (rosuvastatin), dropped from $5.78 per pill to just $0.08 after multiple generics hit the market. That’s a 99% price drop.Combination Pills: One Pill, Two Drugs, Big Savings
If you’re taking two separate generic pills every day, you might be paying more than you need to. Combination products-single pills that contain two medications-often cost less than buying each drug separately. Take asthma or COPD inhalers. Before generics arrived, Advair Diskus cost around $334 per inhaler. When the generic Wixela Inhub hit the market, the price dropped to $115. That’s a 66% savings per prescription. And because Wixela combines fluticasone and salmeterol in one device, patients no longer had to buy two separate inhalers. The total U.S. spending on these two drugs dropped from $337 million per month to $233 million in just one year. The same pattern shows up in other areas. For diabetes, a combination pill with metformin and sitagliptin (like Janumet) often costs less than buying metformin and sitagliptin as separate pills. For high blood pressure, a single pill with amlodipine and olmesartan can be cheaper than buying each drug alone. Pharmacists and doctors don’t always bring this up-but it’s worth asking: “Is there a combination version of these two drugs?”Therapeutic Substitution: Same Result, Lower Price
Sometimes, the best savings don’t come from switching to another version of the same drug. They come from switching to a different drug entirely-one that works just as well but costs far less. This is called therapeutic substitution. The JAMA Network Open study found that 62% of high-cost generics could be replaced with a lower-cost alternative in the same drug class. For example, if you’re taking a high-priced generic statin like rosuvastatin, your doctor might switch you to atorvastatin, which has the same cholesterol-lowering effect but costs a fraction as much. This isn’t theoretical. A 2023 analysis of prescriptions filled through the Mark Cuban Cost Plus Drug Company showed that patients saved an average of $4.96 per prescription. For uninsured people, the average saving was over $6 per fill. And in 28% of cases, savings were over $10 per prescription. That’s $300+ a year just from smarter prescriptions. The key? Your doctor and pharmacist need to know what’s available. The FDA’s Orange Book lists which generics are therapeutically equivalent. Look for an “A” rating-it means the drug is approved as interchangeable with the brand-name version. But don’t assume your prescription is the cheapest option. Ask: “Is there a cheaper generic or alternative that works just as well?”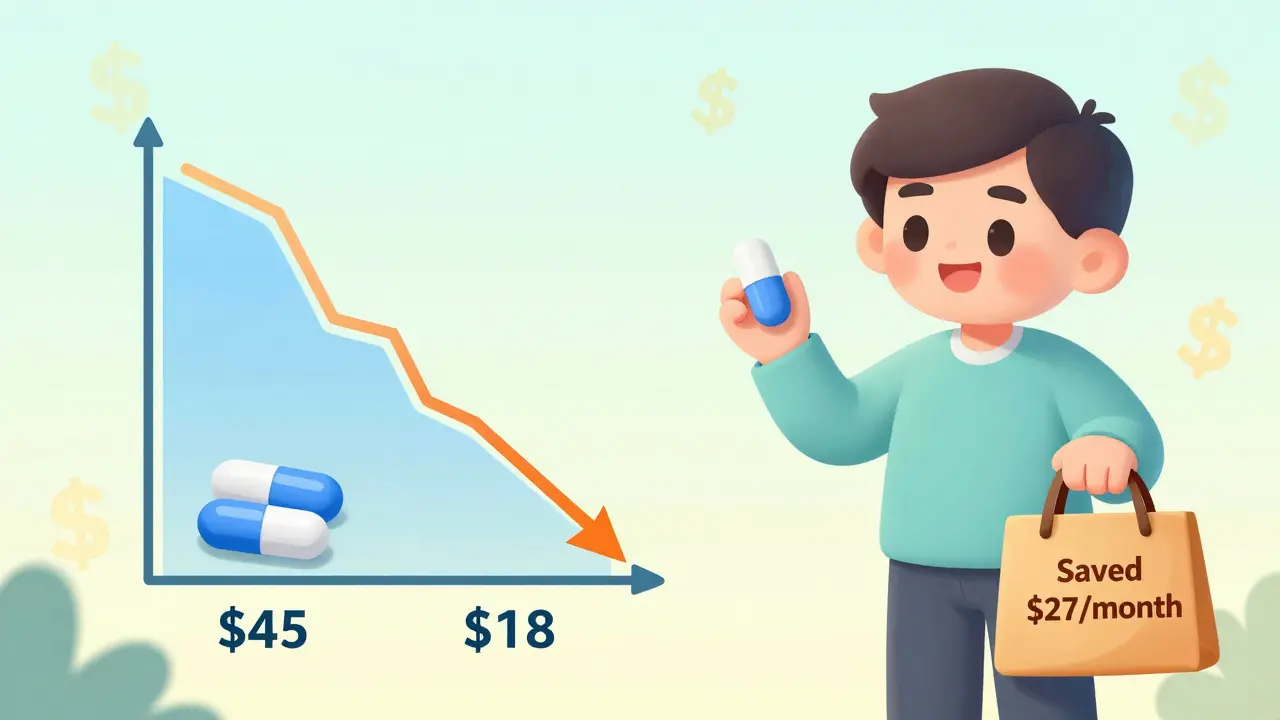
Who Benefits the Most?
The biggest savings go to people without insurance. In one study, 28.9% of uninsured patients saw cost reductions on generic prescriptions, compared to just 5.5% of Medicare users and 7.1% of those with private insurance. Why? Insurance plans often have fixed copays. If your copay is $10, it doesn’t matter if the drug costs $1 or $10-you still pay $10. But for the uninsured, every dollar counts. That’s why services like Mark Cuban’s drug company and community pharmacies offering $4 generics have become lifelines. Medicaid patients saw almost no savings in the same study, because Medicaid already negotiates very low prices. But even they can benefit from combination pills-switching from two separate Medicaid-covered drugs to one combination pill can reduce administrative costs and simplify treatment.How to Find These Savings Yourself
You don’t need a degree in pharmacology to save money. Here’s how to start:- Check your prescriptions. Are you taking two or more pills for the same condition? Ask if a combination version exists.
- Ask your pharmacist. Say: “Is there a cheaper generic version of this drug?” or “Is there another drug in the same class that costs less?”
- Use price comparison tools. Websites like GoodRx, SingleCare, and Blink Health let you compare prices at nearby pharmacies. Sometimes the same drug costs $2 at one store and $40 at another.
- Request a formulary check. If you’re on Medicare or private insurance, ask your plan if they have a preferred generic list. They often have tiered pricing-choose the lowest tier.
- Don’t assume your doctor knows. Many doctors don’t track generic pricing. Bring up cost concerns directly. You’re not being difficult-you’re being smart.
Why This Isn’t Happening More Often
Despite the clear savings, many patients still pay more than they need to. Why? Three big reasons:- Market consolidation. A handful of companies control most of the generic drug market. With fewer competitors, prices stay high.
- Patent tricks. Some brand-name companies pay generic makers to delay cheaper versions-called “pay-for-delay” deals. These are illegal, but they still happen.
- Formulary inertia. Insurance plans stick with the same drugs for years, even when cheaper options appear. They don’t update their lists often enough.
The Bigger Picture
Over the past decade, generic drugs have saved the U.S. healthcare system $3.7 trillion. In 2023 alone, the top 10 generics saved $89.5 billion. That’s money that went back into patients’ pockets, employers’ budgets, and government programs. But the system is fragile. Generic drug shortages have doubled since 2012. Supply chain issues, manufacturing problems, and lack of profit incentives mean some essential drugs are disappearing. Still, the opportunity is real. Every time you choose a lower-cost generic or combination product, you’re not just saving money-you’re helping keep the system sustainable. The data doesn’t lie: smarter choices = big savings. And you don’t need to wait for a policy change to make it happen.Are all generic drugs the same price?
No. Two generics with the same active ingredient can cost very different amounts. One might be made by a company with little competition, while another is made by five companies fighting for market share. The cheaper version is often just as safe and effective. Always ask your pharmacist about lower-cost alternatives.
Can I ask my doctor to switch me to a cheaper generic?
Yes, and you should. Doctors are focused on effectiveness, but cost matters too. Say something like, “I’m trying to lower my medication costs-is there a cheaper generic or combination pill that works just as well?” Most doctors are open to it, especially if you show them price options from GoodRx or your pharmacy.
Are combination pills as safe as taking two separate pills?
Yes. Combination pills are FDA-approved and contain the same active ingredients as the separate versions. They’re often easier to take, reduce pill burden, and improve adherence. The only risk is if you need to adjust the dose of one component-then a separate pill might be better. But for most people, combinations are a safe and smart choice.
Why doesn’t my insurance cover the cheaper generic?
Your plan may not have updated its formulary (list of covered drugs) in a while. Some plans lock in older generics even when cheaper ones become available. Call your insurance provider and ask if they cover a specific generic or combination drug. If they say no, request a formulary exception. Many plans approve these if you provide evidence of cost savings.
How much can I realistically save by switching generics?
It varies. For some drugs, you could save 90% or more-like switching from a $7.50 generic to a $0.50 version. For others, the savings might be $5-$10 per prescription. But if you take multiple meds, those savings add up fast. One study found that 28% of patients saved over $10 per prescription. That’s $120+ a year per drug. Multiply that by three or four prescriptions, and you’re talking about $500+ in annual savings.







Comments(10)