Hashimoto’s thyroiditis isn’t just another thyroid issue. It’s the most common reason people in places like Australia, the U.S., and Europe end up with hypothyroidism - and it’s not caused by diet, stress, or lack of sleep. It’s your own immune system attacking your thyroid. If you’ve been told your TSH is high but you still feel tired, cold, or foggy, this is likely why.
What Exactly Is Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis, first described in 1912 by Japanese doctor Hakaru Hashimoto, is an autoimmune disease where your body mistakes thyroid tissue for a threat. Immune cells - mainly T-cells - invade your thyroid, slowly destroying the cells that make thyroid hormone. Over time, your thyroid can’t keep up, and hormone levels drop. That’s when symptoms like fatigue, weight gain, dry skin, and brain fog show up.
It’s not rare. About 1 in 50 people have it, but among women over 50, that number jumps to 1 in 10. Women are 10 times more likely to get it than men. And while it can show up at any age, it most often starts between 30 and 50.
The real clue? Antibodies. Over 90% of people with Hashimoto’s have thyroid peroxidase antibodies (TPOAb). About two-thirds also have thyroglobulin antibodies (TgAb). These aren’t just markers - they’re proof your immune system is actively attacking your thyroid. A simple blood test can detect them.
How Hashimoto’s Progresses - And Why TSH Matters
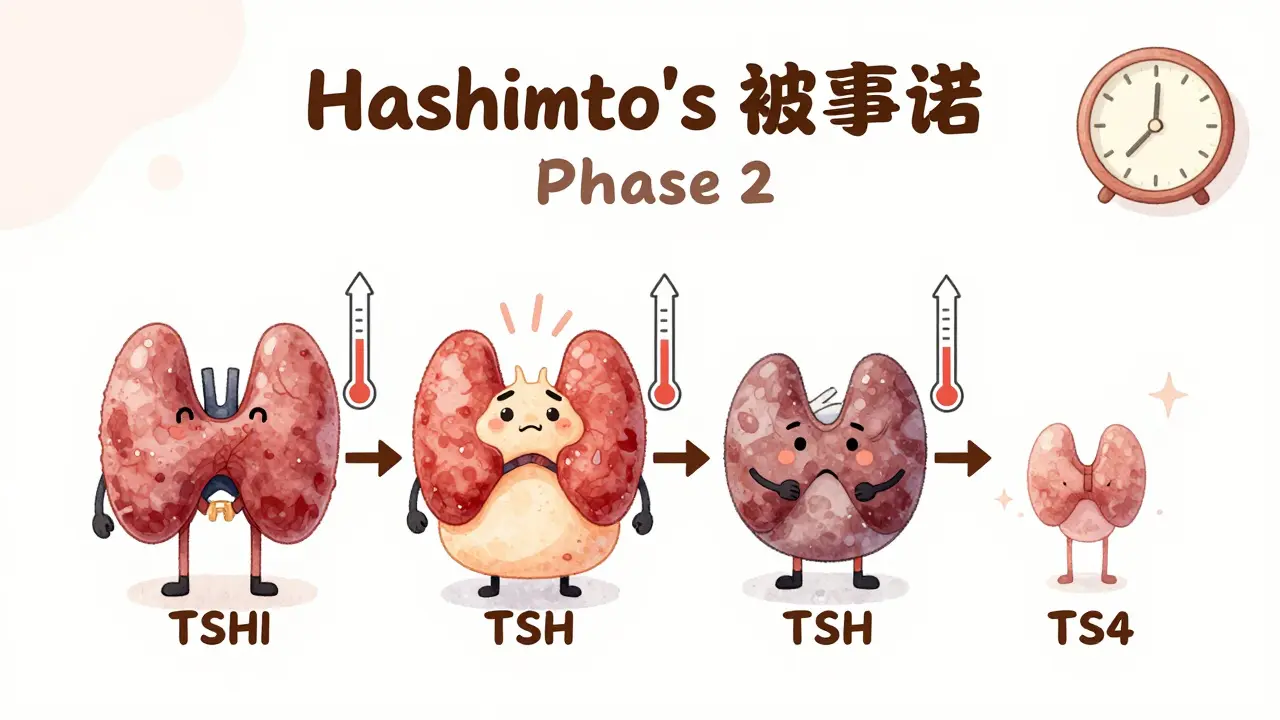
This disease doesn’t hit you all at once. It moves in stages:
- Phase 1: Euthyroid - Your thyroid still works fine. TSH is normal. But antibodies are already high. You might feel fine - or you might have subtle symptoms like mild fatigue.
- Phase 2: Subclinical hypothyroidism - TSH starts creeping up, usually between 4.5 and 10 mIU/L. Free T4 is still normal. This is where many people get diagnosed. Doctors often wait to treat unless symptoms are clear.
- Phase 3: Overt hypothyroidism - TSH goes above 10 mIU/L, and free T4 drops. Symptoms become obvious: weight gain, depression, constipation, hair loss, cold intolerance. This is when levothyroxine is almost always started.
- Phase 4: Atrophy - The thyroid shrinks. The goiter (swelling) you might’ve had earlier disappears. Antibodies may stay high, but the immune attack slows down.
TSH - thyroid stimulating hormone - is your body’s main warning system. It’s made by the pituitary gland and tells the thyroid: “Make more hormone.” When thyroid hormone drops, TSH rises. That’s why TSH is the first test doctors check.
But here’s the catch: TSH alone isn’t always enough.
Why TSH Can Be Misleading - And What to Do About It
Some people have normal TSH levels but still feel awful. Why? Because TSH can be thrown off by antibodies, timing, or other factors.
First, antibody interference. In 5-10% of cases, TSH antibodies bind to the lab equipment and make TSH look higher than it really is. That’s why doctors should also check free T4 if symptoms don’t match TSH.
Second, timing matters. TSH levels rise naturally at night and drop in the morning. Testing after taking your thyroid pill? That can drop TSH by 15-20%. Always test before your morning dose. And wait 24 hours after taking biotin supplements - they can cause false TSH readings up to 30% off.
Third, seasons affect TSH. In colder months, TSH averages 1.8 mIU/L higher than in summer. If your TSH jumps in winter, it might not mean you need more medication - just wait until spring to retest.
And then there’s hashitoxicosis. About 15-20% of people with Hashimoto’s go through a brief hyperthyroid phase early on. The immune attack causes the thyroid to leak stored hormone. You might feel anxious, have heart palpitations, lose weight - and think you have Graves’ disease. But it’s temporary. Within weeks or months, the thyroid burns out and you flip into hypothyroidism. This is why some people need multiple dose adjustments in their first year.
Levothyroxine: The Standard Treatment - And Its Limits
Levothyroxine (T4) is the gold standard. It replaces what your thyroid can’t make anymore. Most people feel better once their TSH is in range. But not everyone.
Here’s what you need to know:
- Dosing starts low - usually 25-50 mcg per day, especially for older adults or those with heart issues. Increase by 12.5-25 mcg every 6-8 weeks until TSH stabilizes.
- Take it empty stomach - at least 30-60 minutes before food or coffee. Calcium, iron, soy, and even high-fiber meals can block absorption. If you take a calcium supplement, wait 4 hours.
- Brand consistency matters - The FDA classifies levothyroxine as a narrow therapeutic index drug. That means even small changes in absorption (5-10%) can throw off your levels. Stick to one brand - whether it’s Synthroid or a generic - and don’t switch unless your doctor says so.
- It’s not a cure - You’ll likely need it for life. But with the right dose, most people live normally.
Still, 10-15% of patients feel tired, depressed, or foggy even with a “normal” TSH. Some doctors try adding T3 (liothyronine) to boost energy. But a major 2017 meta-analysis of 87% of patients showed no real benefit over T4 alone. The American Association of Clinical Endocrinologists doesn’t recommend combination therapy unless TSH stays high after 6 months of optimal T4 dosing.
Real People, Real Challenges
Online communities like Reddit’s r/Hashimotos and the American Thyroid Association’s patient forum are full of stories:
- 68% of 1,247 surveyed patients needed 3 or more dose changes before feeling right.
- 42% went through wild swings - feeling hyper one month, hypo the next - during early treatment.
- 57% of users said their TSH fluctuated despite taking pills daily.
- Triggers? Stress (41%), gluten (32%), and seasonal changes (27%) were top reasons.
One woman in Sydney told her endocrinologist her TSH kept rising every winter. She switched from taking her pill at night to taking it first thing in the morning, stopped eating soy yogurt with breakfast, and started testing at 8 a.m. - not 10 a.m. - after 24 hours without biotin. Her TSH dropped from 7.2 to 2.1 in 3 months.
It’s not magic. It’s precision.
Who Needs Special TSH Targets?
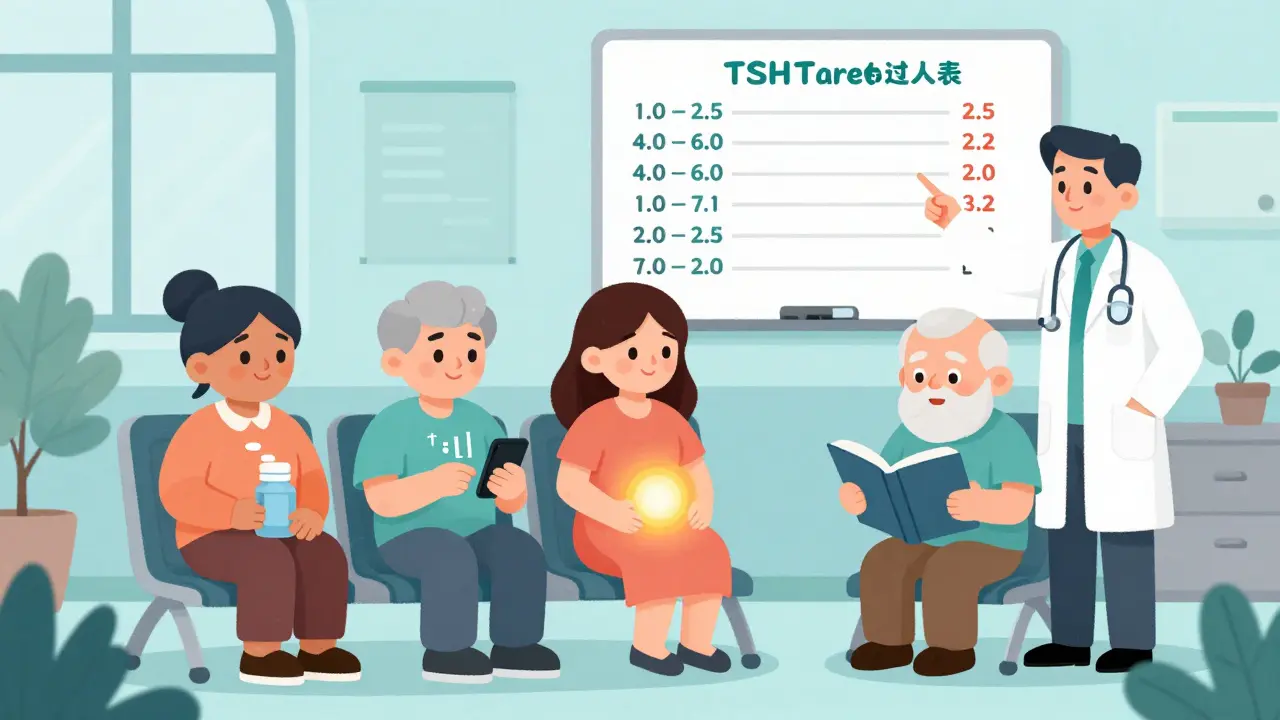
TSH isn’t one-size-fits-all. Your ideal range depends on your life stage.
- Adults under 60: Target TSH 1.0-2.5 mIU/L. Lower is better if you’re still symptomatic.
- Adults over 80: Target TSH 4.0-6.0 mIU/L. Higher TSH is safer to avoid heart strain.
- Pregnant women: TSH must be under 2.5 mIU/L in the first trimester. Above that, miscarriage risk jumps 2.3 times. Dose often needs to increase by 25-30% in early pregnancy.
- People with heart disease: Go slow. Rapid TSH drops can trigger arrhythmias.
Dr. Rebecca Bahn from Mayo Clinic says: “We don’t treat numbers. We treat people.” If you’re tired with a TSH of 3.8, don’t wait until it hits 5. Adjust.
What’s Next? The Future of Hashimoto’s Treatment
Right now, we manage Hashimoto’s by replacing hormone. But research is looking at stopping the attack.
Scientists are studying drugs that calm overactive T-cells - especially those targeting CD4+ pathways. Twelve phase II trials are underway, with results expected by 2028. If they work, we might one day prevent thyroid destruction instead of just replacing what’s lost.
Also, genetic testing is coming. Polymorphisms in genes like CTLA-4 and PTPN22 are linked to worse outcomes. By 2030, doctors may use your DNA to predict how aggressive your Hashimoto’s will be - and set personalized TSH targets before symptoms even start.
For now, though, the best tool is still TSH testing - done right, at the right time, with the right context.
Key Takeaways for Managing Hashimoto’s
- Hashimoto’s is an autoimmune disease - your immune system attacks your thyroid.
- Positive TPOAb confirms the diagnosis in most cases.
- TSH is your main guide, but don’t ignore symptoms or free T4 if something feels off.
- Test TSH in the morning, before your pill, and 24 hours after biotin.
- Levothyroxine is effective for most - take it on an empty stomach, consistently.
- Seasons, stress, and gluten can trigger TSH swings. Track your patterns.
- Dose adjustments take 6-8 weeks to stabilize. Don’t rush.
- Target TSH varies by age, pregnancy, and health history - don’t aim for the same number as someone else.
Hashimoto’s isn’t a death sentence. It’s a condition you can manage - if you understand how your body responds, how your meds work, and when to push for better answers.




Comments(8)