Lupus Cardiovascular Risk Calculator
This tool estimates your cardiovascular risk based on lupus-specific factors and traditional risk factors. Enter your information to calculate your risk score.
Enter your information to see your risk assessment.
Living with lupus (systemic lupus erythematosus) means dealing with a disease that can touch almost every organ. One area that often catches people off guard is the heart and blood vessels. Understanding how lupus interacts with the cardiovascular system helps you spot warning signs early, work with your doctor on the right plan, and keep your heart beating strong.
What "lupus" Really Means for the Heart
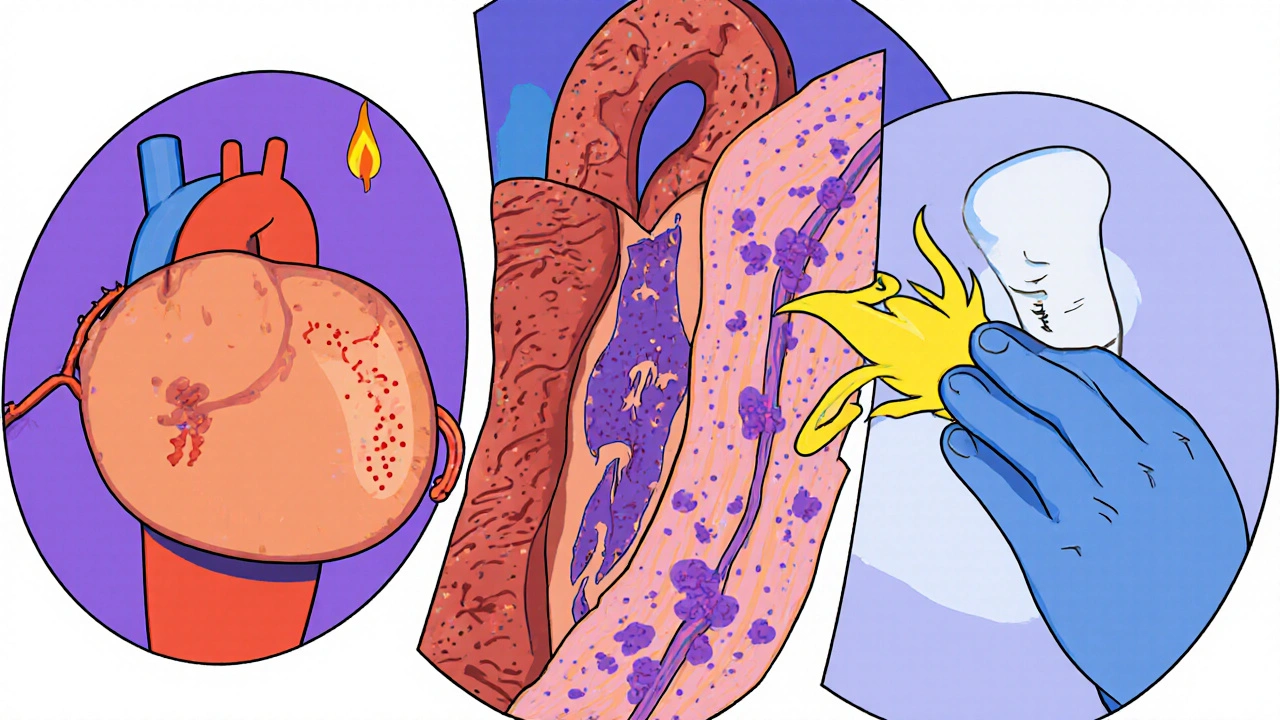
Systemic Lupus Erythematosus is an autoimmune disease where the immune system mistakenly attacks healthy tissue, causing inflammation across the body. When that inflammation reaches the heart or blood vessels, the fallout can range from mild chest discomfort to life‑threatening events. The key point is that lupus doesn’t just sit in the joints-it can silently damage the arteries, the lining of the heart, and the tiny vessels that feed nerves and muscles.
The Most Common Cardiovascular Problems in Lupus
- Pericarditis is inflammation of the sac around the heart, often causing sharp chest pain that eases when you sit up.
- Myocarditis is inflammation of the heart muscle itself, which can lead to fatigue, shortness of breath, or abnormal heart rhythms.
- Atherosclerosis accelerates in lupus patients, meaning plaque builds up faster and raises the risk of heart attacks and strokes.
- Antiphospholipid syndrome (APS) creates a clotting tendency that can block arteries or veins, causing deep‑vein thrombosis or pulmonary embolism.
- Raynaud's phenomenon causes the fingers and toes to turn white or blue in cold, reflecting the same blood‑vessel spasms that can affect coronary arteries.
Why Lupus Increases Cardiovascular Risk
Three main mechanisms drive the higher heart risk:
- Chronic inflammation - The immune system constantly releases cytokines that irritate the inner lining of arteries (endothelial dysfunction), making them sticky and prone to plaque.
- Autoantibodies - Antibodies like anti‑double‑stranded DNA and antiphospholipid antibodies directly attack blood‑vessel components.
- Medication side effects - Long‑term use of high‑dose corticosteroids can raise blood pressure and cholesterol, while some immunosuppressants may affect lipid profiles.
The combination of these forces means the lupus cardiovascular risk is several times higher than in age‑matched people without lupus.
Spotting the Red Flags Early
Because lupus can sneak up on the heart, learning the symptoms is vital. Call your doctor if you notice:
- Sharp, stabbing chest pain that worsens when lying down (possible pericarditis). \n
- Unexplained fatigue, breathlessness, or swelling in the ankles (could be myocarditis or heart failure).
- Sudden palpitations or fainting spells (arrhythmias).
- Persistent coldness or color change in fingers/toes (Raynaud's signaling vessel issues).
- Leg pain, swelling, or redness that comes on quickly (sign of a clot, think APS).
Routine monitoring-blood pressure checks, lipid panels, and echocardiograms-helps catch problems before they become emergencies.
How Doctors Diagnose Lupus‑Related Heart Issues
The diagnostic toolkit blends standard heart tests with lupus‑specific labs:
| Test | What It Shows | Why It Matters |
|---|---|---|
| Electrocardiogram (ECG) | Heart rhythm and electrical activity | Detects arrhythmias, pericarditis changes |
| Echocardiogram | Heart structure and motion | Finds pericardial effusion, myocarditis, valve issues |
| Cardiac MRI | Detailed tissue characterization | Identifies inflammation, scar tissue |
| Blood tests (CRP, ESR) | Inflammation levels | Correlates active lupus with heart risk |
| Antiphospholipid antibody panel | Presence of lupus‑related clotting antibodies | Guides anticoagulation therapy |
| Lipid profile | Cholesterol and triglycerides | Helps manage atherosclerosis risk |
Managing the Cardiovascular Threat
Treatment is a blend of controlling lupus activity and protecting the heart. Here’s a practical roadmap:
- Keep lupus quiet - Disease‑modifying drugs like hydroxychloroquine have been shown to lower flare rates and may reduce heart‑attack risk.
- Watch steroids - Use the lowest effective dose; taper quickly when possible to avoid high blood pressure and cholesterol spikes.
- Address traditional heart risk factors - Adopt a Mediterranean‑style diet, aim for regular moderate exercise, quit smoking, and keep blood pressure below 130/80 mm Hg.
- Medications for the vessels - Statins can slow atherosclerosis; low‑dose aspirin or anticoagulants may be prescribed for APS.
- Regular screening - Annual ECG and echocardiogram for those with persistent symptoms, plus yearly lipid and glucose checks.
Working closely with a rheumatologist and a cardiologist is the safest way to balance immune suppression with heart protection.
Lifestyle Tips That Make a Difference
Small daily habits can tip the scales in your favor:
- Stay active - 30 minutes of brisk walking most days improves circulation and lowers cholesterol.
- Control stress - Mind‑body practices like yoga or meditation can dampen inflammatory cytokines.
- Watch sodium - High salt pushes blood pressure up, especially if steroids are part of your regimen.
- Get enough sleep - Poor sleep heightens inflammation; aim for 7‑8 hours.
- Monitor weight - Even modest weight loss can improve heart‑health markers.
What the Latest Research Says
Recent studies (2023‑2025) are sharpening our view of lupus‑heart connections. A 2024 multinational cohort of 2,500 lupus patients found that those on hydroxychloroquine had a 30 % lower incidence of myocardial infarction compared with those not on the drug. Another 2025 trial showed that low‑dose colchicine reduced pericarditis recurrence by half.
Scientists are also exploring the role of the complement system-a part of innate immunity-in driving endothelial damage. Early‑phase drugs that block complement C5 are showing promise in reducing vascular inflammation, which could become a future option for high‑risk lupus patients.
When to Seek Emergency Care
Some situations demand immediate attention:
- Sudden, crushing chest pain lasting more than a few minutes.
- Severe shortness of breath with rapid heartbeat.
- Loss of consciousness or sudden weakness on one side of the body.
- Swelling in the legs that worsens quickly, suggesting heart failure.
Dial emergency services right away-time is heart muscle.
Can lupus cause a heart attack?
Yes. Lupus accelerates atherosclerosis and can trigger clotting disorders, both of which raise heart‑attack risk.
Is pericarditis a sign of a lupus flare?
Often. In many patients, new chest pain with a pericardial rub signals active disease and needs prompt treatment.
Do steroids always hurt the heart?
Not always, but high doses over long periods raise blood pressure and cholesterol. Doctors aim for the lowest dose that controls lupus.
Should I take daily aspirin?
Aspirin may help if you have antiphospholipid antibodies, but only take it under medical advice because of bleeding risk.
How often should I get a heart scan?
If you have cardiac symptoms or high lupus activity, an echocardiogram every year is common. Otherwise, a baseline scan after diagnosis and follow‑up every 2-3 years often suffices.
Takeaway Checklist
- Know the five key heart problems linked to lupus.
- Track blood pressure, cholesterol, and lupus activity regularly.
- Ask your doctor about hydroxychloroquine and low‑dose statins if you’re at risk.
- Adopt heart‑healthy lifestyle habits-exercise, diet, stress control.
- Seek emergency care for sudden chest pain or severe shortness of breath.
Understanding the link between lupus and the cardiovascular system turns a scary unknown into a manageable part of your health plan. With the right tests, medicines, and everyday habits, you can protect your heart while living with lupus.





Comments(11)