Dose-Related Side Effects: How Medication Amounts Impact Your Safety
When you take a medicine, the amount matters just as much as the drug itself. This is called dose-related side effects, adverse reactions caused by the quantity of a medication rather than its chemical identity. Also known as dosage toxicity, it’s not about being allergic—it’s about how your body handles too much, too little, or the wrong timing of a drug. A pill that helps one person might hurt another, not because of genetics or allergies, but because the dose was too high for their size, age, or kidney function.
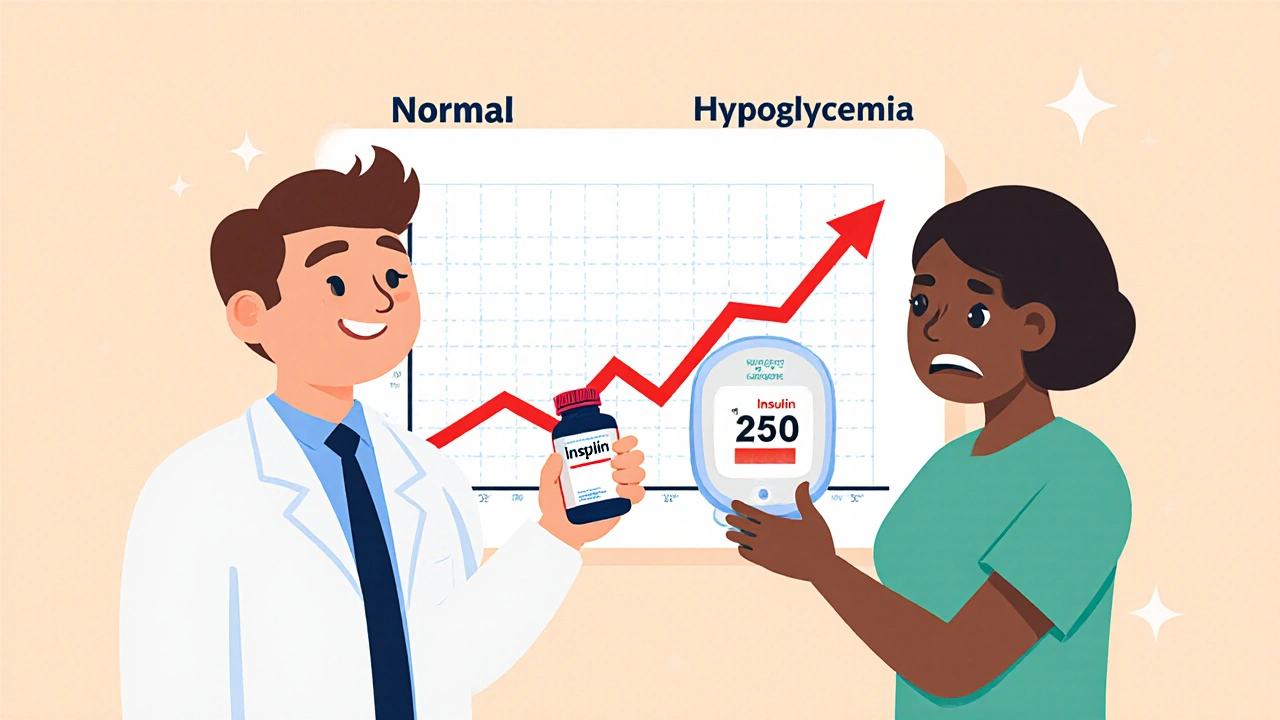
Therapeutic window, the range between the minimum effective dose and the minimum toxic dose. Also known as safe dosage range, it’s the sweet spot where a drug works without causing harm. Many drugs—like warfarin, lithium, or digoxin—have a narrow window. Go a little over, and you risk bleeding, seizures, or heart rhythm problems. Go under, and the drug does nothing. This is why restarting a medication after a break can be deadly: your body loses tolerance, and the dose that once felt fine now feels overwhelming. That’s why overdose prevention, strategies to avoid harmful drug levels due to reduced tolerance or drug interactions. Also known as medication restart safety, it’s critical for opioids, benzodiazepines, and even antidepressants. The same goes for older adults, people with kidney disease, or those on multiple drugs. A common painkiller like diclofenac might seem harmless, but at high doses or with other NSAIDs, it can trigger stomach bleeds or kidney damage. Even CBD oil, often seen as safe, can block liver enzymes and cause your other meds to build up to dangerous levels.
Some drugs are designed to hit specific targets, like lowering urate below 6 mg/dL in gout. Too little, and flares keep coming. Too much, and you risk side effects like liver stress or skin reactions. That’s why urate targets, specific blood levels of uric acid used to guide gout treatment. Also known as serum urate goals, they’re not guesses—they’re evidence-based thresholds. Same with bicarbonate in chronic kidney disease: too little, and acid builds up and speeds up kidney damage. Too much, and you get fluid overload or high blood pressure. It’s not about taking more—it’s about taking the right amount for your body right now.
And it’s not just about pills. Drug interactions can change how your body processes a dose. Take tizanidine with ciprofloxacin, and your blood pressure can crash. Mix dofetilide with cimetidine, and your heart rhythm goes haywire. These aren’t rare accidents—they’re predictable, preventable, and often missed because no one checked what else you’re taking. Your pharmacist doesn’t just count pills—they track how doses interact, how age changes metabolism, and how your DNA affects absorption. That’s why pharmacogenomics, using your genes to predict how you’ll respond to medications. Also known as personalized dosing, it’s turning guesswork into science.
What you’ll find below are real stories from people who learned the hard way: why restarting an antidepressant after a month off nearly killed someone, how a simple switch from retail to hospital pharmacy changed a patient’s outcome, and why a dose that worked for years suddenly stopped working—or started hurting. These aren’t theoretical warnings. They’re lessons from patients, doctors, and pharmacists who’ve seen the consequences of ignoring dose-related risks. Whether you’re managing gout, kidney disease, heart rhythm issues, or just taking common painkillers, the right dose isn’t on the bottle—it’s in your body, your history, and your other meds. Let’s walk through what you need to know to stay safe.