When your skin breaks out in thick, red, scaly patches, it’s easy to think it’s just a cosmetic issue. But for nearly one in three people with psoriasis, something deeper is happening-something that attacks not just the skin, but the joints too. This is psoriatic arthritis (PsA), a real, painful, and often misunderstood autoimmune disease that doesn’t wait for permission to spread. It’s not just "bad eczema" or "old age aches." It’s your immune system turning on your own body, and if left unchecked, it can cause permanent joint damage.
How Psoriasis Turns Into Psoriatic Arthritis
Psoriasis starts as plaques-raised, inflamed patches covered in silvery scales-usually on elbows, knees, scalp, or lower back. About 80 to 90% of people with psoriasis have this form. But for 6% to 39% of them, the inflammation doesn’t stop at the skin. It moves into the joints. That’s psoriatic arthritis. Most of the time, psoriasis shows up first. In fact, 85% of people with PsA had skin symptoms before their joints started hurting. But in 5 to 10% of cases, the joint pain comes first. That’s when things get tricky. Doctors might mistake it for rheumatoid arthritis or just general wear and tear. Without knowing about the hidden psoriasis, diagnosis gets delayed. And every month without treatment means more damage. The trigger? It’s not one thing. Genetics play a big role. If you have HLA-B27, HLA-B38, or HLA-B39 genes, your risk goes up. But genes alone don’t cause it. Stress, infections, injury, or even gut bacteria changes can flip the switch. Your immune system starts attacking healthy tissue-skin cells multiply too fast, and joint linings swell up. It’s like your body’s alarm system is stuck on fire.The Five Signs You Might Have Psoriatic Arthritis
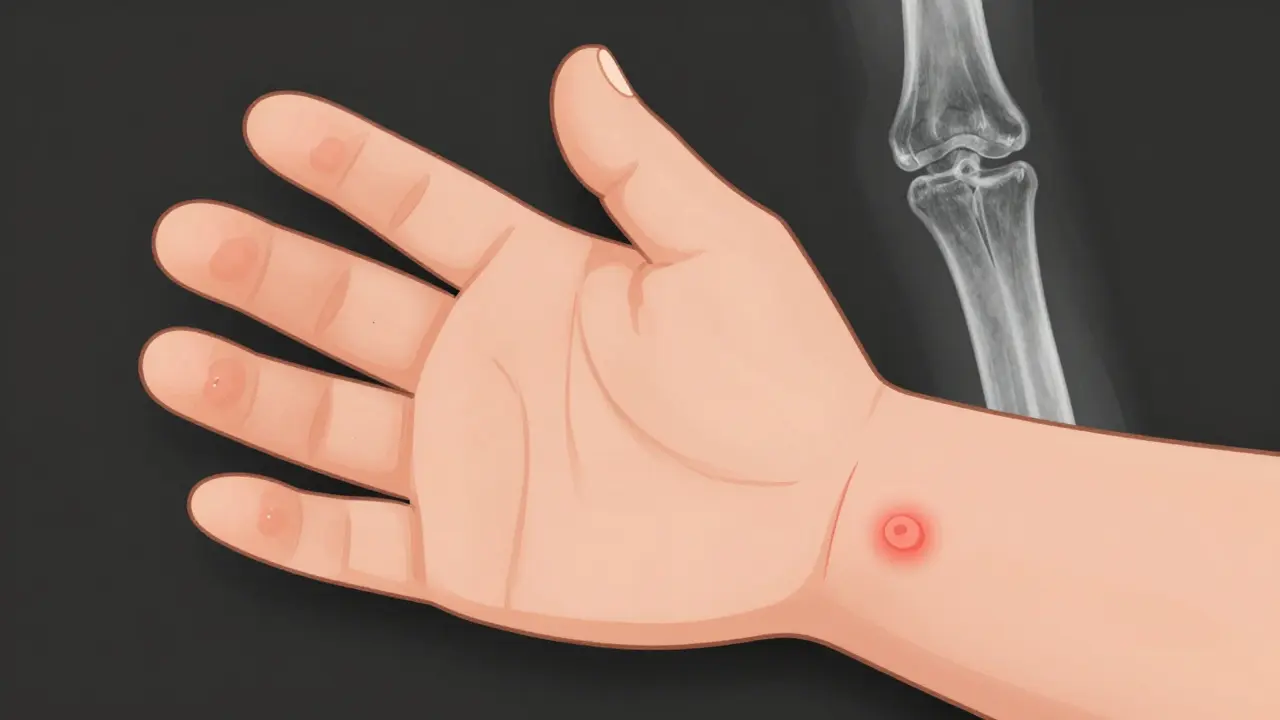
PsA doesn’t look the same in everyone. But there are five clear patterns doctors look for:- Dactylitis: One or more fingers or toes swell up like sausages. It’s not just a sore joint-it’s the whole digit, inflamed from tip to base. Around 40% of people with PsA get this.
- Enthesitis: Pain where tendons or ligaments attach to bone. Think Achilles tendon pain or the bottom of your foot. It’s common in 35 to 50% of cases.
- Nail changes: Pitting, crumbling, or nails lifting off the nail bed. About 80% of PsA patients have this. Many assume it’s a fungal infection, but it’s often the first sign of something deeper.
- Asymmetric joint pain: Unlike rheumatoid arthritis, which usually hits both sides equally, PsA often affects just one knee, one wrist, or one finger. It’s unpredictable.
- Back and spine pain: If your lower back or neck stiffens up, especially in the morning, and improves with movement, it could be axial PsA. This affects the spine and sacroiliac joints.
And here’s something many don’t realize: you can have all these signs and still test negative for rheumatoid factor. That’s a key clue. Rheumatoid arthritis usually shows up in blood tests. PsA often doesn’t.
How Doctors Diagnose It
There’s no single blood test for PsA. Diagnosis relies on connecting the dots. The gold standard is the CASPAR criteria-a checklist doctors use to confirm it. You need inflammatory joint disease plus at least three of these:- Current or past psoriasis (3 points)
- Psoriatic nail changes (1 point)
- Negative rheumatoid factor (1 point)
- Dactylitis (1 point)
- Typical bone changes on X-ray (1 point)
A score of 3 or higher? That’s PsA. But getting there takes time. Doctors will review your medical history, check your skin and joints, order blood tests for inflammation markers like CRP and ESR, and likely order imaging. X-rays show bone damage, but MRIs and ultrasounds catch early swelling before bones get hurt. A skin biopsy might be done to rule out other conditions like eczema or fungal infections.
Many people wait years before getting diagnosed. That’s dangerous. The earlier you catch it, the more damage you can prevent.
What Happens If You Don’t Treat It
PsA isn’t just about pain. It’s about long-term harm. Without treatment, up to 70% of people develop bone erosion. In 30 to 40%, you’ll see “pencil-in-cup” deformities-where bone dissolves on one side and grows abnormally on the other. Joints can fuse. Fingers can bend permanently. Spinal mobility can shrink. But the damage isn’t just physical. People with PsA have a 43% higher risk of heart attack. Around half also have metabolic syndrome-high blood pressure, belly fat, high blood sugar. Depression and anxiety are twice as common. Quality of life scores drop by 30 to 40% compared to healthy peers. Mortality rates are 30 to 50% higher, mostly because of heart disease. This isn’t a skin condition you can ignore. It’s a whole-body disease. Treating the rash alone won’t save your joints or your heart.Treatment: From Pain Relief to Stopping the Attack
Treatment isn’t one-size-fits-all. It’s based on how bad it is and which parts of your body are affected. For mild cases, over-the-counter NSAIDs like ibuprofen help with pain and swelling. But they don’t stop the disease. If it’s more serious, doctors turn to DMARDs. Methotrexate, taken weekly, is common. It slows the immune system’s attack. But it’s slow-takes months to work. For moderate to severe PsA, biologics are the game-changer. These are targeted drugs that block specific parts of the immune system:- TNF inhibitors (like adalimumab, etanercept): Best for spine and tendon pain. About half of patients see a 20% improvement (ACR20), and 30-40% see 50% improvement (ACR50).
- IL-17 inhibitors (secukinumab, ixekizumab): Better for skin and nails. Often clear up plaques faster than TNF blockers.
- IL-12/23 inhibitors (ustekinumab): Good for both skin and joints.
- JAK inhibitors (tofacitinib): Oral pills that block inflammation signals inside cells.
There’s a new wave of drugs coming. Drugs like guselkumab (targeting IL-23) and deucravacitinib (a TYK2 inhibitor) are already approved and showing strong results. Bimekizumab, which blocks both IL-17A and IL-17F, is proving even more effective for skin and joint symptoms.
Doctors now aim for minimal disease activity-not just less pain, but near-normal function. That means:
- 1 or fewer tender or swollen joints
- Psoriasis covering 1% or less of skin
- Pain score under 15 out of 100
- Ability to do daily tasks without struggle
- No fatigue
If you hit these targets, your risk of long-term damage drops dramatically.

The Gut-Skin-Joint Connection
New research is pointing to your gut. Studies show people with PsA have different gut bacteria than those without it. Some types of bacteria are missing. Others are overgrown. This might explain why some people flare after antibiotics or a high-sugar diet. Scientists are now testing probiotics, fiber-rich diets, and even fecal transplants to see if rebalancing gut microbes can calm inflammation. It’s early, but it’s promising. What you eat might not cure PsA-but it could help you stay in remission longer.What You Can Do Today
You can’t change your genes. But you can change how you live:- Get checked: If you have psoriasis and joint pain, don’t wait. See a rheumatologist.
- Track your symptoms: Keep a journal. When does pain flare? What foods or stressors make it worse?
- Move regularly: Low-impact exercise like swimming, cycling, or yoga keeps joints flexible and reduces stiffness.
- Quit smoking: Smoking makes PsA worse and cuts the effectiveness of biologics.
- Watch your weight: Extra pounds put more stress on joints and increase inflammation.
- Check your heart: Get blood pressure, cholesterol, and blood sugar checked yearly. PsA raises your risk-you need to manage it like a heart condition.
PsA is not a death sentence. But it demands attention. The tools to control it are better than ever. The key is catching it early and treating it like the systemic disease it is-not just a skin problem.
What’s Next
By 2027, experts predict 70% of PsA patients will be on advanced therapies within two years of diagnosis-up from 40% today. That’s because we now know: early, aggressive treatment saves joints, organs, and lives. New biomarkers-like calprotectin and MMP-3-are being tested to predict who will respond to which drug. Imagine a blood test that tells you whether adalimumab or secukinumab will work best for you. That’s the future. The goal isn’t just to manage symptoms. It’s to stop the disease before it starts.Can psoriasis cause joint pain even if my skin looks fine?
Yes. While most people develop skin symptoms first, 5 to 10% of those with psoriatic arthritis experience joint pain before any visible rash appears. This can delay diagnosis, as doctors may not suspect PsA without skin signs. If you have unexplained joint swelling, stiffness, or pain-especially in fingers, toes, or the lower back-and a family history of psoriasis, get evaluated by a rheumatologist.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both cause joint inflammation, rheumatoid arthritis (RA) usually affects joints symmetrically and often shows positive rheumatoid factor in blood tests. Psoriatic arthritis (PsA) is asymmetric, commonly affects the spine and tendons, and typically has negative rheumatoid factor. PsA also includes skin and nail changes, which RA doesn’t. The CASPAR criteria help doctors tell them apart.
Can diet cure psoriatic arthritis?
No diet can cure PsA. But some people find that reducing sugar, processed foods, and alcohol helps lower inflammation. A diet rich in omega-3s (like fatty fish), vegetables, and fiber may improve symptoms and support gut health, which is linked to PsA flare-ups. Always combine dietary changes with medical treatment-don’t replace medication with food alone.
Do biologics have serious side effects?
Biologics suppress parts of the immune system, so they can increase the risk of infections like tuberculosis or fungal infections. Before starting, you’ll be screened for latent TB and hepatitis. Rarely, they may be linked to nervous system disorders or certain cancers. But for most people, the benefits far outweigh the risks-especially since untreated PsA carries higher risks of heart disease, joint destruction, and early death. Regular monitoring helps catch issues early.
Will I need to take medication forever?
For most people, yes. PsA is a chronic condition. Stopping treatment often leads to flare-ups and increased joint damage. Some people in deep remission may reduce doses under doctor supervision, but stopping entirely is risky. The goal is long-term control-not a cure. Think of it like managing high blood pressure: you take medicine to prevent damage, even when you feel fine.
Can children get psoriatic arthritis?
Yes. Although rare, children can develop psoriatic arthritis, often after psoriasis appears. In kids, it may present as dactylitis or enthesitis more than classic joint swelling. Early diagnosis is critical to prevent growth problems and joint deformities. Pediatric rheumatologists specialize in treating children with PsA and tailor treatments to their needs.







Comments(14)