Renal Dosing Calculator for Metformin and SGLT2 Inhibitors
How to Use This Calculator
Enter your patient's eGFR value (mL/min/1.73 m²) to see appropriate dosing recommendations for metformin and SGLT2 inhibitors based on current 2026 guidelines.
Important: This tool reflects the most recent guidelines (KDIGO 2022, ADA 2024). Always verify with current prescribing information and clinical judgment.
Enter eGFR Value
Key Clinical Considerations
Important Note: eGFR may dip 2-5 mL/min/1.73 m² when starting SGLT2 inhibitors. This is typically a transient hemodynamic effect, not kidney damage.
When eGFR drops below 30: Metformin should be avoided entirely (unless in specific stable patients with close monitoring).
eGFR 20-29 range: SGLT2 inhibitors can be used, but metformin should be stopped.
Dosing Recommendations
Metformin Recommendations
Enter eGFR value to see recommendations
SGLT2 Inhibitor Recommendations
Enter eGFR value to see recommendations
When to Adjust Metformin and SGLT2 Inhibitors for Kidney Function
If you’re managing type 2 diabetes and have chronic kidney disease (CKD), your medication plan needs to change as your kidneys slow down. This isn’t just a minor tweak-it’s a critical safety step. Too much metformin when your kidneys can’t clear it properly can lead to lactic acidosis, a rare but dangerous condition. Meanwhile, SGLT2 inhibitors like dapagliflozin and empagliflozin can protect your kidneys, but only if dosed right. The rules changed in 2022, and many doctors are still catching up. Here’s what actually matters today.
Metformin: The Old Rules Are Out
For years, metformin was stopped completely if your eGFR dropped below 60 mL/min/1.73 m². That changed after a 2016 FDA safety update and a wave of new data showing metformin’s benefits outweigh the risks-even in moderate kidney disease. Now, you can still take it, but you must reduce the dose.
- eGFR ≥60: Max dose is 2550 mg per day.
- eGFR 45-59: Max dose drops to 2000 mg per day.
- eGFR 30-44: Max dose is 1000 mg per day.
- eGFR <30: Avoid metformin entirely. Some clinicians may use 500 mg daily in stable patients, but this is off-label and requires close monitoring.
Why the change? A 2014 BMJ study found lactic acidosis from metformin occurs in only 3.3 cases per 100,000 patient-years-far lower than once thought. Meanwhile, metformin cuts heart attacks and death in people with diabetes and kidney disease. Stopping it unnecessarily does more harm than good.
SGLT2 Inhibitors: Kidney Protection Starts Earlier
SGLT2 inhibitors-drugs like dapagliflozin (Farxiga), empagliflozin (Jardiance), and canagliflozin (Invokana)-aren’t just blood sugar pills. They’re kidney protectors. The 2022 KDIGO guidelines, backed by trials like DAPA-CKD and EMPA-KIDNEY, lowered the minimum eGFR for starting these drugs from 30 to 20 mL/min/1.73 m². That’s a big deal.
These drugs reduce the risk of kidney failure, heart attack, and death by 30-40% in people with CKD. That’s why guidelines now say: start them early. You don’t wait until your kidneys are failing. You start when you have albuminuria (protein in urine) and eGFR ≥20, even if your blood sugar is under control.
Here’s how dosing breaks down by drug:
- Canagliflozin: Max 100 mg/day if eGFR is 45-59. Not recommended below 45.
- Dapagliflozin: Max 10 mg/day if eGFR is 25-45. Contraindicated below 25.
- Empagliflozin: Max 10 mg/day if eGFR is 30-45. Contraindicated below 30.
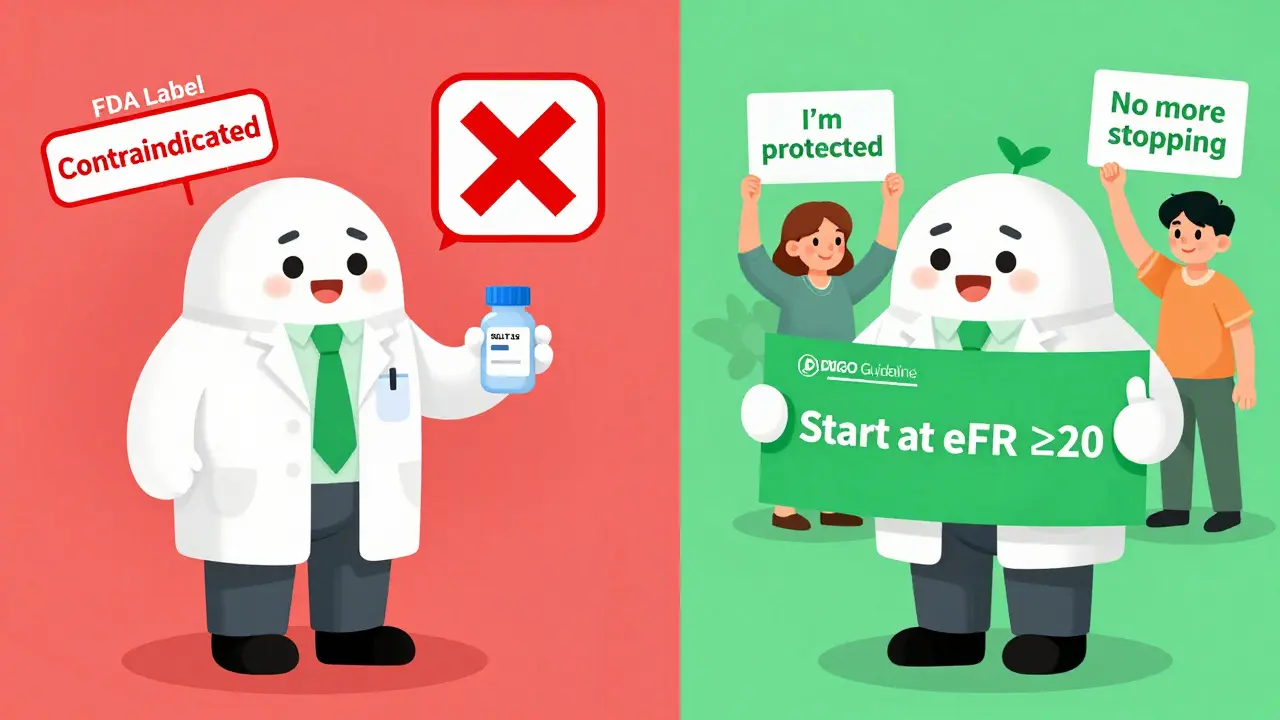
But here’s the twist: once you start an SGLT2 inhibitor, you can keep taking it even if your eGFR drops below 20, as long as you’re not having side effects or starting dialysis. This is a major shift. Many doctors still panic when eGFR falls and stop the drug. Don’t. That dip? It’s often temporary.
The eGFR Dip: Don’t Panic
When you start an SGLT2 inhibitor, your eGFR often drops by 2-5 mL/min/1.73 m² in the first few weeks. This isn’t kidney damage-it’s a normal hemodynamic effect. The drug reduces pressure in the kidney’s filtering units, which actually protects them long-term.
The UK Kidney Association says it clearly: “A decline in eGFR needs to be interpreted with caution and in the context of an expected drug effect.” I’ve seen patients drop from 32 to 27, then bounce back to 30 by month 3. Their proteinuria dropped 40%. Stopping the drug would’ve cost them kidney protection.
Check your eGFR 4-6 weeks after starting. If it’s stable or rebounding, keep going. If it keeps falling fast-like more than 10 points in 3 months-then investigate for other causes: dehydration, heart failure, or another kidney problem.
Combining Metformin and SGLT2 Inhibitors
For most people with type 2 diabetes and CKD, the best first combo is metformin plus an SGLT2 inhibitor. The ADA and KDIGO both recommend this as early as possible.
But there’s a narrow gap: eGFR 20-29 mL/min/1.73 m². In this range:
- You can start or keep an SGLT2 inhibitor (per KDIGO).
- You should stop metformin (per ADA and Diabetes Canada).
That means if your eGFR is 25, you’re on metformin 1000 mg, and you add dapagliflozin-you need to stop the metformin. It’s counterintuitive, but the risk of lactic acidosis rises as eGFR drops below 30, even if you’re on a low dose. The kidney protection from the SGLT2 inhibitor alone is enough.
What About Dialysis?
There’s no clear consensus for patients on dialysis. Metformin is mostly cleared by the kidneys, and dialysis removes it, but not perfectly. Some sources suggest 250 mg daily for peritoneal dialysis and 500 mg after hemodialysis. But this is low-quality evidence. Most guidelines say: avoid.
SGLT2 inhibitors? They’re not approved for dialysis patients. Their mechanism relies on functioning kidney tubules to block glucose reabsorption. If your kidneys are gone, the drug doesn’t work. Don’t use them.
Monitoring: How Often to Check
Renal dosing isn’t a one-time decision. You need ongoing checks.
- eGFR ≥60: Check every 6-12 months.
- eGFR 45-59: Check every 3-6 months.
- eGFR 30-44: Check every 3 months.
- Starting or changing SGLT2 inhibitor: Check eGFR and sodium at 2-4 weeks.
Also, watch for signs of volume depletion: dizziness, low blood pressure, dry mouth. These are more common in older adults or those on diuretics. If you’re sick-vomiting, diarrhea, fever-hold your SGLT2 inhibitor for a few days. That’s the “sick-day rule.”
The Regulatory Mess
Here’s where things get messy. The FDA hasn’t caught up with the science.
Canagliflozin’s FDA label still says: contraindicated if eGFR <45. But KDIGO says: start it at eGFR ≥20. That’s a direct conflict.
Many insurers deny coverage for SGLT2 inhibitors when eGFR is 20-29 because the FDA label says “no.” A 2022 ADA survey found 43% of endocrinologists had prescriptions denied for this reason. Patients get stuck. Doctors choose between following guidelines or risking insurance rejection.
Dr. Katherine Tuttle, lead author of the KDIGO 2022 update, says: “Clinicians should follow evidence-based clinical practice guidelines rather than regulatory labeling when they conflict.” That’s the reality. You’re not breaking the law-you’re using the best available science.
What’s Next?
The FDA approved dapagliflozin for kidney disease even without diabetes in February 2024. That’s huge. But their label still says eGFR ≥25. KDIGO recommends down to 20. The gap is still there.
Draft guidelines from ADA and KDIGO for 2025 are already looking at use in eGFR 15-19. Early data suggests benefits persist even there. The future is clear: SGLT2 inhibitors will become standard for almost all CKD patients with proteinuria-diabetic or not.
Metformin’s role will shrink in advanced CKD, but it’ll stay first-line for mild to moderate disease. The key is matching the drug to the kidney, not the other way around.





Comments(14)