Statin Intolerance Assessment Tool
Understand Your Symptoms
This tool helps determine if your muscle symptoms are likely related to statins. Based on the National Lipid Association criteria, 80% of people labeled as "intolerant" can actually tolerate statins after proper evaluation.
Your Assessment
Results will appear here after assessment.
Next Steps
Your personalized recommendations will appear here.
For millions of people taking statins to lower cholesterol and prevent heart attacks, muscle pain isn't just an inconvenience-it's a dealbreaker. Many stop their medication because of discomfort, thinking they're intolerant. But what if the problem isn't the drug itself, but how it was managed? Statin intolerance clinics are changing that. These specialized programs don't just label patients as "intolerant." They dig deeper, test smarter, and find ways to keep people on life-saving therapy.
What Really Counts as Statin Intolerance?
Statin intolerance isn't a one-size-fits-all diagnosis. The National Lipid Association updated its definition in 2022 to reflect a spectrum: it's not just about pain. It's about symptoms that clearly link to statin use and go away when you stop taking it. The old rule-needing to fail two statins-has been replaced with a more practical approach. If you have muscle aches, weakness, or cramps that start within weeks of starting a statin and vanish after stopping, that's the red flag.Here's the catch: not everyone who feels sore is truly intolerant. Studies show that up to 80% of people who think they can't take statins might be able to-once you rule out other causes. That's why clinics don't just take your word for it. They run tests. They look at thyroid function. They check vitamin D levels. They review every supplement you're taking, including CoQ10 or red yeast rice. Sometimes, the real culprit is a drug interaction or an underactive thyroid, not the statin.
The Four-Step Protocol That Works
Statin intolerance clinics follow a strict, evidence-based process. It’s not guesswork. It’s a step-by-step system that’s been proven across major health systems like Cleveland Clinic and Kaiser Permanente.- Stop the statin. You’ll stop taking it completely for two full weeks. No partial doses. No switching brands. Just stop.
- Monitor symptoms. During those two weeks, you keep a simple diary: rate your pain on a scale of 0 to 10, note when it’s worst, and track whether it improves. If your symptoms fade, that’s a strong clue the statin was the trigger.
- Rule out other causes. Blood tests check for thyroid issues, kidney function, and elevated creatine kinase (CK). A CK level over 10 times the normal limit is a major red flag. But even if your CK is normal, symptoms alone can still point to statin intolerance.
- Rechallenge smartly. This is where most clinics succeed. Instead of trying the same statin again, they switch to one with a different profile. Hydrophilic statins like rosuvastatin or pravastatin are less likely to enter muscle tissue. Many patients tolerate these just fine-even at low doses.
Some patients then move to intermittent dosing: taking rosuvastatin just twice a week. A 2021 Cleveland Clinic study of over 1,200 patients found that 76% of those previously labeled intolerant could stay on this schedule without pain. Their LDL cholesterol dropped by 20-40%-enough to cut heart attack risk significantly.
Why Switching Statins Makes a Difference
Not all statins are created equal. Lipophilic statins like simvastatin and atorvastatin easily slip into muscle cells, which may explain why they cause more muscle-related side effects. Hydrophilic statins like rosuvastatin and pravastatin are designed to be pulled into the liver, not the muscles. This small difference matters a lot.Clinics use this knowledge strategically. If a patient had trouble with simvastatin, they don’t just try another lipophilic statin like atorvastatin. They go straight to rosuvastatin 5 mg twice a week. The success rate? Around 72%. That’s not luck-it’s science.
Even better, some patients who couldn’t tolerate daily dosing do fine with every-other-day or twice-weekly regimens. The liver still gets enough statin to lower LDL, but muscles get less exposure. This approach works especially well for older adults and those with kidney issues, where statin clearance is slower.
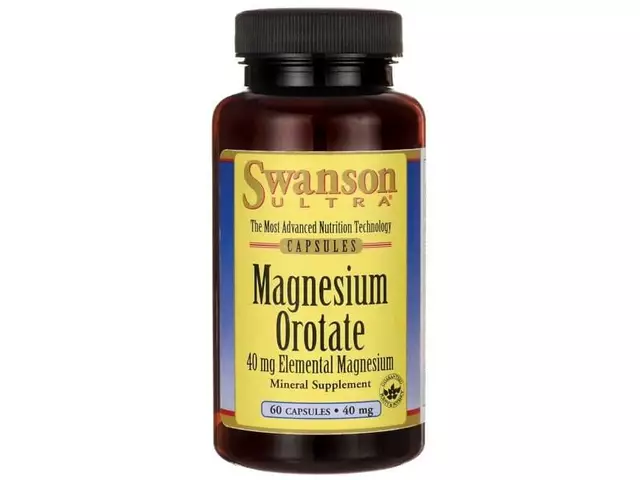
What If You Still Can’t Tolerate Statins?
For the 10-15% who truly can’t take any statin-even at low or intermittent doses-there are proven alternatives. The first-line option is ezetimibe. It’s not flashy, but it’s affordable ($35 a month) and proven. The IMPROVE-IT trial showed it reduces heart attacks and strokes by 6% when added to statins. For people who can’t take statins at all, it’s a solid foundation.Another option is bempedoic acid (Nexletol). Approved in 2020, it lowers LDL by about 18% without causing muscle pain. Unlike statins, it works in the liver and doesn’t affect muscle tissue. It costs more-around $491 a month-but for patients at high risk, it’s often worth it. In the CLEAR Outcomes trial of over 14,000 people, bempedoic acid didn’t cause muscle symptoms even in those who’d previously failed statins.
PCSK9 inhibitors like evolocumab are powerful-they can slash LDL by 60%-but they’re expensive ($5,850 a year) and often denied by insurers. Many clinics help patients appeal these denials. One patient on Inspire shared that it took 11 weeks and four appeals to get coverage. But for someone with familial hypercholesterolemia or a history of heart attack, it can be life-saving.
Real Results from Real Clinics
Numbers don’t lie. At Cleveland Clinic, 68% of patients in their statin intolerance program reached their LDL-C goal. At Kaiser Permanente, 82% of patients in their program got back on lipid-lowering therapy-compared to just 45% in regular care. That’s a huge difference.One patient, "HeartPatient87," shared on Reddit: "After being told I was statin intolerant for five years, Johns Hopkins put me on rosuvastatin 5 mg twice a week with CoQ10. My LDL dropped from 142 to 89. No pain. No more fear." That’s the kind of outcome these clinics are designed for.
Meanwhile, clinics that skip the structured approach often miss the mark. A 2017 study found that 45% of patients who were told they were intolerant by general practitioners permanently quit statins. In clinics using protocols, that number dropped to 18%. The difference? Systematic evaluation.

Barriers and What’s Next
There are still hurdles. Wait times for lipid clinics can be 6-8 weeks. Insurance companies still fight coverage for non-statin drugs. And some patients are afraid to rechallenge-even when it’s safe.But change is coming. The ACC launched its Statin Intolerance Tool in March 2023, giving doctors a step-by-step digital guide to assess risk and make decisions. Mayo Clinic started genetic testing for SLCO1B1 variants in 2023-this gene can predict who’s at higher risk for simvastatin muscle damage. And new nanoparticle statin formulations are in early trials, showing 92% tolerability.
By 2024, 78% of lipid specialists plan to expand intermittent dosing. More health systems are adopting protocols. The American Heart Association reports that 63 of the top 100 U.S. health systems now have formal statin intolerance programs. Academic centers lead the way-87% have protocols-while community hospitals are catching up.
What You Can Do Today
If you’ve been told you’re statin intolerant:- Don’t assume you’ll never take one again.
- Ask your doctor about a lipid clinic referral.
- Keep a symptom diary before and after stopping the statin.
- Request a CK test and thyroid panel.
- Ask about switching to rosuvastatin or pravastatin.
- Consider intermittent dosing-even once or twice a week can work.
- If you can’t take statins, ask about ezetimibe or bempedoic acid.
Statins cut heart attacks and strokes by 20-25% for every 1 mmol/L drop in LDL. That’s not optional. For millions, the solution isn’t quitting statins-it’s finding the right way to take them.
What is the difference between statin intolerance and statin side effects?
Statin side effects are temporary discomforts that may happen to anyone, like mild muscle soreness after starting a new dose. Statin intolerance is diagnosed when symptoms are consistent, recur with re-exposure, and disappear after stopping the drug. It’s not about occasional discomfort-it’s about a clear pattern that prevents safe, ongoing use.
Can I just stop taking statins if I feel muscle pain?
No. Stopping statins without evaluation increases your long-term risk of heart attack or stroke. Muscle pain could be caused by something else-like low vitamin D, thyroid issues, or overexertion. A structured clinic will help you find the real cause before you quit.
Is rosuvastatin better than atorvastatin for people with muscle pain?
Yes, for many. Rosuvastatin is hydrophilic, meaning it’s mainly absorbed by the liver and less likely to enter muscle tissue. Atorvastatin is lipophilic and can spread into muscles more easily. Switching from atorvastatin to rosuvastatin is one of the most successful strategies in statin intolerance clinics, with a 72% success rate in restoring tolerance.
How often should I take statins if I’m on an intermittent schedule?
Most patients start with rosuvastatin 5 mg twice a week (e.g., Monday and Thursday). Some do well with once-weekly dosing. The goal is to maintain LDL-lowering while minimizing muscle exposure. Your lipid specialist will adjust based on your cholesterol levels and symptoms.
Are non-statin therapies as effective as statins?
Not always-but they can be very effective. Ezetimibe reduces LDL by 15-20% and cuts cardiovascular events by 6%. Bempedoic acid lowers LDL by 18% without muscle side effects. PCSK9 inhibitors can drop LDL by 60%. While statins remain the gold standard, these alternatives offer real protection for those who truly can’t tolerate them.
Why do some doctors say statin intolerance is overdiagnosed?
Because of the nocebo effect. When patients expect side effects, they’re more likely to notice and report them. Studies using blinded rechallenge-where patients don’t know if they’re taking the statin or a placebo-show that up to 80% of people who think they’re intolerant actually tolerate statins when they don’t know they’re taking them. That’s why structured clinics use objective testing, not just patient reports.
Statin intolerance clinics aren’t about giving up on statins. They’re about finding the path back to them-safely, effectively, and permanently.




Comments(13)