Sjögren’s Syndrome isn’t just about being thirsty or having watery eyes. It’s when your immune system turns on the very glands that keep you moist - the ones that make tears, saliva, and other fluids. Imagine your body’s natural lubricants suddenly shutting down. That’s what happens in Sjögren’s. It doesn’t just cause discomfort - it changes how you eat, sleep, work, and even connect with others. And yet, most people have never heard of it.
More than 4 million Americans live with this condition, and about 9 out of 10 are women. The average age of diagnosis is 48. But here’s the problem: it takes nearly three years on average for someone to get a correct diagnosis. Doctors often mistake it for allergies, stress, aging, or even dehydration. By the time it’s confirmed, the damage to glands and other organs may already be underway.
What Happens Inside Your Body?
Your body has glands - tiny factories - that produce moisture. The lacrimal glands make tears. The salivary glands make saliva. When you blink, your eyes stay wet. When you chew, saliva helps you swallow. In Sjögren’s, your immune system sends white blood cells to attack these glands. They don’t just slow down production - they destroy them.
This isn’t limited to your eyes and mouth. The same attack can spread to other moisture-producing tissues: the skin, the vagina, the lungs, even the kidneys. About half of women with Sjögren’s experience vaginal dryness. One in five develop a persistent dry cough from lung involvement. Skin becomes flaky, itchy, and cracked. Nerves can get damaged, leading to numbness or tingling in hands and feet.
It’s not just about dryness. Fatigue hits like a wall. Not the kind you can fix with sleep. This is bone-deep exhaustion that makes getting out of bed feel impossible. Brain fog is common - forgetting words mid-sentence, struggling to focus in meetings. Many patients say their cognitive struggles are worse than the physical symptoms.
Why Is It So Hard to Diagnose?
There’s no single test for Sjögren’s. Doctors look for a mix of symptoms, lab results, and physical signs. The American College of Rheumatology requires at least three months of persistent dry eyes and dry mouth, plus one or more objective findings:
- Tear production below 5mm in 5 minutes (Schirmer’s test)
- Saliva flow under 1.5mL in 15 minutes
- Presence of anti-SSA/Ro or anti-SSB/La antibodies in blood (found in 60-70% of cases)
- Biopsy showing lymphocyte clusters in minor salivary glands
Even then, it’s tricky. Some people have all the symptoms but test negative for antibodies. Others have the antibodies but no symptoms. That’s why many patients see four or more doctors before getting answers. One Reddit user visited an ENT, a dentist, a primary care doctor, and an allergist - each blaming something else. It wasn’t until a rheumatologist ordered a lip biopsy that the diagnosis clicked.
Ultrasound of the salivary glands is now used more often. In 2022, the European League Against Rheumatism updated guidelines to include it, because it’s 85% accurate at spotting inflammation - without needing a biopsy.
It’s Not Just Dryness - It’s Systemic
Many people think Sjögren’s is just a dry mouth and dry eyes condition. That’s a dangerous myth. It’s a full-body autoimmune disease. About 30-50% of patients also have another autoimmune disorder - usually rheumatoid arthritis or lupus. That’s called secondary Sjögren’s.
But even in primary Sjögren’s (where it stands alone), the immune system doesn’t stop at glands. Joint pain is common - not like arthritis that destroys bones, but more like constant aching that moves around. Up to 70% of patients report debilitating fatigue. Some develop lung scarring, kidney problems, or nerve damage. A small percentage - about 4-5% over a lifetime - develop non-Hodgkin lymphoma, a type of cancer that starts in immune cells. That’s why regular monitoring matters.
Unlike lupus, which attacks skin, kidneys, and brain all at once, Sjögren’s starts in the glands. But over time, it can follow a similar path. That’s why experts call it the “great imitator.” It looks like fibromyalgia, like chronic fatigue syndrome, like menopause, like stress. But it’s not any of those. It’s an autoimmune attack - and it needs different treatment.
What Treatments Actually Work?
There’s no cure. But there are ways to manage it - and some new options are finally emerging.
For dry eyes, preservative-free artificial tears are the first line. You might need them 8-10 times a day. Some patients use tiny silicone plugs in the tear ducts to keep tears from draining too fast. For dry mouth, saliva substitutes help - but they’re temporary. Prescription drugs like pilocarpine (5mg three times daily) or cevimeline can stimulate saliva production. Around 60-70% of people report noticeable improvement.
Dental care becomes critical. With less saliva, cavity risk jumps 5-10 times higher. Patients need checkups every 3-4 months, not every six. Fluoride treatments, xylitol gum, and avoiding sugary drinks are non-negotiable.
For systemic symptoms - joint pain, fatigue, inflammation - hydroxychloroquine (Plaquenil) is often prescribed. It helps about 30-40% of people. For those with severe inflammation or organ involvement, newer biologics are being tested. In June 2023, the FDA approved Efgartigimod (Vyvgart Hytrulo), the first new Sjögren’s treatment in 20 years. In trials, it improved dry mouth symptoms by 35% compared to placebo.
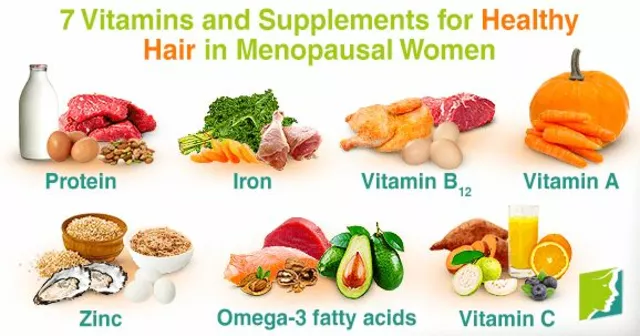
Complementary therapies are common. A 2022 patient survey found 89% use special oral care products, 52% take omega-3 supplements, and 23% try acupuncture. While not cures, many report reduced discomfort.
Life With Sjögren’s: The Hidden Costs
The financial toll is heavy. Annual healthcare costs for someone with Sjögren’s average $12,500 - nearly three times higher than for someone their age without it. Dental care makes up 35-40% of that. Productivity losses from missed work and reduced performance add another $3.8 billion a year in the U.S. alone.
But the emotional cost is worse. A 2022 survey by the Sjögren’s Syndrome Foundation found 42% of patients showed signs of depression - more than five times the national average. Many feel dismissed. “I told my doctor I couldn’t swallow my toast,” one patient wrote. “She said, ‘Just drink more water.’”
Relationships suffer. Vaginal dryness is rarely discussed, but it’s real. One woman on MySjogrensTeam said it took 18 months to find a gynecologist who understood it was part of her autoimmune disease - not just “getting older.”
Even simple things become hard. Eating a sandwich. Laughing without choking. Wearing contact lenses. Driving in dry air. These aren’t minor inconveniences. They’re daily battles.

What’s Changing in 2025?
There’s new hope. In 2023, the NIH launched the Sjögren’s Precision Medicine Network, enrolling 5,000 patients across 25 centers to match treatments to individual biomarkers. Researchers have identified a T-cell signature present in 78% of patients - a potential diagnostic tool.
The TARGET initiative, a $15 million research program, is now hunting for genetic markers that predict who will develop severe symptoms. That could lead to earlier, personalized treatment.
Twelve new therapies are in clinical trials. Three target B-cells - the immune cells that go rogue in Sjögren’s. One, a biosimilar of rituximab, showed promise in reducing fatigue and joint pain.
Medical education is catching up. The American Medical Association added Sjögren’s modules to its continuing education platform in 2022. Over 45,000 doctors have now been trained to recognize it.
But awareness still lags. Research funding is shockingly low. In 2022, the NIH spent $28.7 million on Sjögren’s. For lupus? $167 million. For rheumatoid arthritis? $114 million. Yet Sjögren’s affects more people than both combined.
What You Can Do Right Now
If you’ve had dry eyes and dry mouth for more than three months - especially if you’re a woman over 40 - don’t wait. See a rheumatologist. Ask for an anti-SSA/SSB blood test. Ask about Schirmer’s test and salivary flow measurement.
Start tracking your symptoms: How often do you need water? Do your eyes burn at the end of the day? Do you wake up with a dry mouth? Is your skin cracking? Write it down. Bring it to your doctor.
Use humidifiers at home and work. Keep humidity between 40-60%. Avoid fans blowing directly on your face. Drink water constantly - not just when you’re thirsty. Use sugar-free gum or lozenges with xylitol to stimulate saliva. Choose soft, moist foods. Avoid alcohol, caffeine, and salty snacks - they dry you out more.
Find a community. Reddit’s r/Sjogrens has 12,500 members. MySjogrensTeam has 25,000. You’re not alone. And you’re not imagining it. Your symptoms are real. Your pain is valid. And help is getting better.





Comments(9)