The skin around your eyes is the thinnest on your entire body-just 0.55 millimeters thick. That’s why even small amounts of everyday cosmetics can trigger a reaction. If you’ve had red, itchy, flaky eyelids that won’t go away, you’re not alone. About 74% of eyelid dermatitis cases are caused by allergic contact dermatitis (ACD), according to a 2023 NIH study. And most people have no idea what’s causing it.
Why Your Eyelids Are So Sensitive
Your eyelids aren’t just delicate-they’re constantly exposed. Every time you apply mascara, wipe your face with a towel, touch your hair after using shampoo, or even apply nail polish and then rub your eyes, you’re transferring potential allergens. The skin there doesn’t have much of a protective barrier, so chemicals slip right in. And because the reaction is delayed, symptoms don’t show up until 24 to 48 hours later. That’s why people often blame their makeup from yesterday, when the real culprit was their nail polish from three days ago.Top 7 Allergens That Trigger Eyelid Dermatitis
Not all cosmetics are created equal when it comes to triggering reactions. Based on a 2021 NIH study of 215 patients, here are the most common offenders:- Nickel (28.7%) - Found in cheap eyeglass frames, eyelash curlers, and even magnetic eyelashes.
- Shellac (21.4%) - The UV-cured gel polish used in manicures. It’s not just on your nails-it’s on your fingers, then your eyelids.
- Preservatives (18.9%) - Especially methylisothiazolinone, parabens, and formaldehyde releasers. These are in almost every cream, serum, and wipe.
- Topical antibiotics (15.3%) - Neomycin and bacitracin are common in eye drops and ointments. Many people think they’re helping, but they’re making things worse.
- Fragrances (14.6%) - Even "natural" or "unscented" products can contain hidden fragrance chemicals.
- Acrylates (12.1%) - Used in long-wear mascaras, waterproof liners, and "smudge-proof" formulas.
- Surfactants (9.8%) - Found in cleansers and makeup removers. They strip the skin and let allergens penetrate deeper.
Here’s the twist: the most common allergens for eyelids are different from those that cause rashes on your arms or neck. Fragrances and preservatives might top the list for general contact dermatitis, but on the eyelids, nickel and shellac are the real troublemakers.
Why Patch Testing Is Non-Negotiable
You can’t guess your way out of this. A 2022 study in the Journal of the American Academy of Dermatology found that patch testing identifies the true cause in 89% of cases when expanded panels are used. Clinical history alone? Only 37% accurate.Patch testing isn’t painful. Small amounts of common allergens are taped to your back for 48 hours. You come back for a reading, and then again a day or two later for a delayed reaction check. The results tell you exactly what to avoid. Dr. Erin Warshaw from Wake Forest puts it bluntly: "If you haven’t had patch testing, you’re just guessing. And guessing means your rash keeps coming back."
Many patients think they’re avoiding makeup, but they’re still using shampoo, hand sanitizer, or nail polish. Dr. Mark G. Rubin of Pure Dermatology says 42% of cases involve indirect exposure-like touching your hair after dyeing it, then rubbing your eyes.
What Happens If You Use the Wrong Cream
It’s tempting to grab a steroid cream from the cabinet. But the eyelids are not the same as your arms. High-potency steroids like clobetasol can cause permanent skin thinning in as few as 7 to 10 applications. Worse, if the cream contains corticosteroid allergens like tixocortol pivalate or budesonide-which some patients react to-it can make things worse.In December 2022, the FDA approved Eysuvis 0.25%, the first steroid ointment specifically designed for eyelid use. Clinical trials showed 89% of patients saw relief within two weeks without eye pressure spikes or cataract risk. But it’s not a cure-it’s a temporary fix while you identify the real trigger.

How to Stop the Reaction for Good
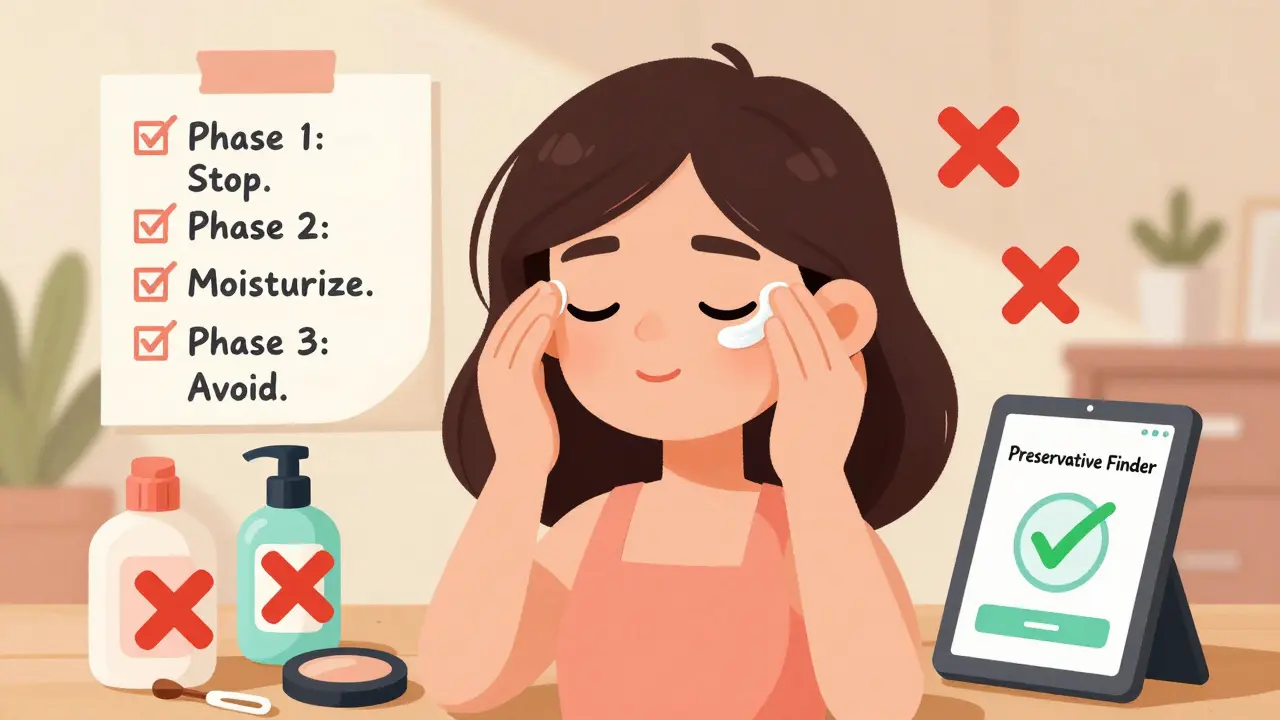
There’s a proven three-phase approach backed by the American Contact Dermatitis Society:- Phase 1 (Days 1-3): Stop everything. No makeup, no eye drops unless prescribed, no new skincare. Use cool compresses to soothe swelling. Wash your hands before touching your face.
- Phase 2 (Days 4-14): Moisturize smartly. Stick to plain petroleum jelly (like Vaseline) or a fragrance-free, preservative-free ointment like CeraVe Healing Ointment. Avoid anything with water in the first five ingredients-water means preservatives.
- Phase 3 (Day 15+): Avoid like your life depends on it. Once you know your allergens, remove them from every product you use. That includes hair dye, nail polish, and even hand soap.
Patients who follow this with a detailed ingredient list have a 68% success rate. Those who just say "I’ll avoid makeup"? Only 32% get better.
Reading Labels Like a Pro
Cosmetic ingredients are listed in INCI (International Nomenclature of Cosmetic Ingredients) format. Here’s what to look for:- Shellac - Look for "Carnauba Wax," "Acrylates," or "UV-cured gel"
- Nickel - Not listed on ingredients, but found in metal eyelash curlers, glasses, and magnetic lashes
- Preservatives - Methylisothiazolinone, methylchloroisothiazolinone, quaternium-15, DMDM hydantoin, imidazolidinyl urea
- Fragrance - "Parfum," "Fragrance," "Essential Oil Blend," "Natural Scent"
- Acrylates - Polyacrylate, PEG-90, methacrylates
There’s a free app called "Preservative Finder" that’s been downloaded over 147,000 times. Just scan a product barcode and it flags 37 known allergens.
The "Transfer Effect" You Didn’t Know About
One of the biggest surprises in patient reports? Nail polish. Women who started wearing gel manicures noticed eyelid swelling within days. They didn’t put polish on their eyes-they just touched their face after applying it. In fact, 71% of nail-related eyelid cases involve women who use gel polish regularly, according to Bennett & Bloom Eye Centers.Same goes for hair dye. If you dye your hair and then rub your eyes, the allergens in the dye (especially paraphenylenediamine) can cause a reaction. Even if you wash your hands, residue stays under your nails.
"Clean Beauty" Isn’t Always Safe
A September 2023 study in JAMA Dermatology found that 33% of "natural" or "organic" eye products contained hidden botanical allergens. Plants from the Compositae family-like chamomile, calendula, and echinacea-are common in "gentle" eye creams but are top triggers for allergic reactions. Just because it’s labeled "natural" doesn’t mean it’s safe for sensitive skin.What to Do Next
If you’ve had eyelid irritation for more than two weeks:- Stop using all eye makeup and non-essential skincare
- Switch to petroleum jelly for moisturizing
- Book a patch test with a board-certified dermatologist
- Download the Preservative Finder app
- Check the Contact Allergen Replacement Database (CARD) for verified safe products
Card, updated monthly by the University of Louisville, lists over 12,800 allergen-free alternatives for everything from mascara to cleansers. You don’t have to give up beauty-you just need to know what to avoid.
Why This Isn’t Just a Skin Problem
Eyelid dermatitis is often a sign of broader sensitization. In 63% of cases, patients react to the same allergens on other parts of their body-like their neck, hands, or ears. That’s why patch testing doesn’t just help your eyelids. It can prevent rashes elsewhere.And the problem is growing. The Global Contact Dermatitis Market reports a 4.7% annual rise in eyelid cases since 2018. Why? Because cosmetic companies keep adding more preservatives, fragrances, and polymers to meet consumer demand for "long-wear," "waterproof," and "natural" products. The EU’s 2023 labeling rules will help, but until then, you have to be your own detective.
Can eyelid dermatitis cause permanent damage?
Yes-if you use high-potency steroid creams for too long. Skin thinning, visible blood vessels, and even changes in eyelash growth can occur after just 7-10 applications of strong steroids like clobetasol. The good news? Stopping the allergen and using the right treatment can reverse most damage within weeks.
Is eyelid dermatitis contagious?
No. It’s not caused by bacteria, viruses, or fungi. It’s an allergic reaction triggered by chemicals in products you use. You can’t catch it from someone else, and you can’t give it to them.
How long does it take to heal?
Most people see improvement within 1-2 weeks of removing the allergen. About 29% need 3-6 weeks, especially if the reaction is chronic or they’ve been using steroids. Full recovery depends on strict avoidance-once you reintroduce the trigger, the rash comes back.
Can I wear makeup again after it clears up?
Yes-but only if you know what caused it. Use the CARD database to find safe alternatives. Start with one product at a time, and wait 72 hours before adding another. Many people find they can wear mascara again, just not the one with shellac or acrylates.
Why do my eyelids get worse in winter?
Dry air cracks the skin barrier, letting allergens penetrate more easily. Plus, people use more heavy creams and occlusive products in winter, which often contain more preservatives. Keep your skin hydrated with plain petroleum jelly and avoid fragranced moisturizers.





Comments(8)