After a colonoscopy finds and removes polyps, many people wonder: when do I need another one? It’s not a one-size-fits-all answer. The timing depends on what kind of polyps were found, how many, how big they were, and how they looked under the microscope. Getting the next colonoscopy too soon wastes time, money, and causes unnecessary stress. Waiting too long could miss a cancer before it’s treatable.
Why the Timing Matters
Not all polyps are the same. Most are harmless, but some can turn into colorectal cancer over 10 to 15 years. The goal of follow-up colonoscopies isn’t to check for the same polyps again - they’re gone. It’s to catch new ones early, before they become dangerous. The latest guidelines, updated in 2020 by the US Multi-Society Task Force on Colorectal Cancer, are built on decades of data showing exactly how risk changes based on polyp features.Here’s the reality: if you had just one or two small adenomas, your cancer risk is almost the same as someone with a completely normal colonoscopy. That’s why the recommended wait time went from 5 years to 7-10 years. But if you had three or more polyps, or any were larger than 10 mm, the clock resets faster.
What Counts as Low Risk?
Low-risk polyps are the most common. They’re usually:- One or two adenomas (precancerous growths)
- Smaller than 10 mm (about the size of a pea)
- With tubular histology (normal cell structure)
- Fully removed in one piece
If your polyps fit this profile, you’re in the low-risk group. The 2020 guidelines say you can safely wait 7 to 10 years before your next colonoscopy. That’s a big change from the old 5-year rule. Studies show people in this group have a 99.3% chance of staying cancer-free at 10 years - nearly identical to those with no polyps at all.
Still, many doctors stick to the old 5-year schedule out of habit or fear of missing something. But research from Oregon Health & Science University shows extending the interval doesn’t increase cancer risk. In fact, it reduces unnecessary procedures by over 30% in this group.
What Triggers a Shorter Wait? 3-Year Rule
If your polyps have any of these features, you need a follow-up in 3 years:- One or more adenomas 10 mm or larger
- Adenomas with villous features (finger-like projections)
- High-grade dysplasia (abnormal cells that are closer to cancer)
- Traditional serrated adenomas (a type of precancerous polyp)
These features mean the polyps were more aggressive or had a higher chance of coming back. A 3-year window lets your doctor check for new growths before they become advanced. Missing this window increases your risk of developing cancer within the next decade.
Also, if you had five or more adenomas - even if they’re small - the 3-year rule applies. The number matters as much as the size.
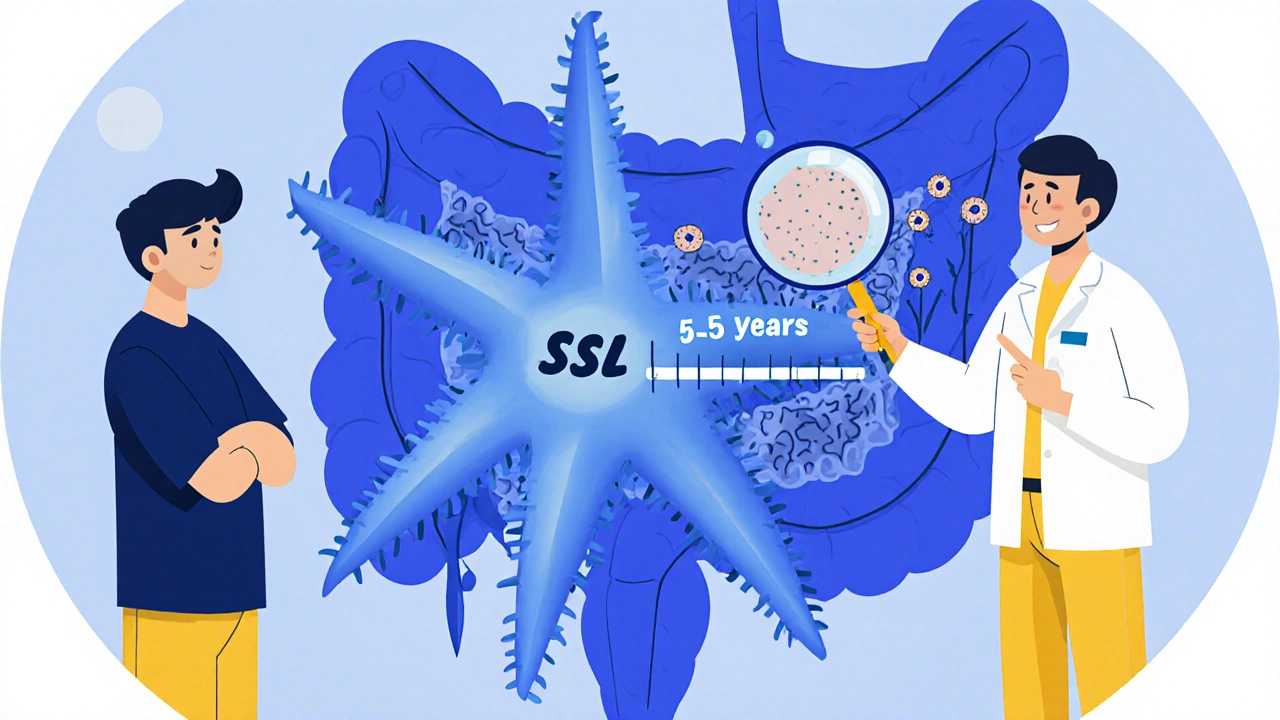
Serrated Polyps: A Different Path
Serrated polyps - especially sessile serrated lesions (SSLs) - are trickier. They don’t look like traditional adenomas. They’re flat, often hidden in folds, and can turn into cancer faster than you’d expect.If you had one or two SSLs smaller than 10 mm, wait 5 to 10 years. But if you had three to four, the next colonoscopy should be in 3 to 5 years. Five or more? Back in 3 years.
Here’s the catch: it’s hard to tell SSLs apart from hyperplastic polyps (HPs), which are usually harmless. If your doctor isn’t sure, or if the polyp was removed in pieces, they’ll recommend a 3-year follow-up just to be safe. Poor bowel prep also pushes the timeline forward - if the colon wasn’t clean enough, something could’ve been missed.
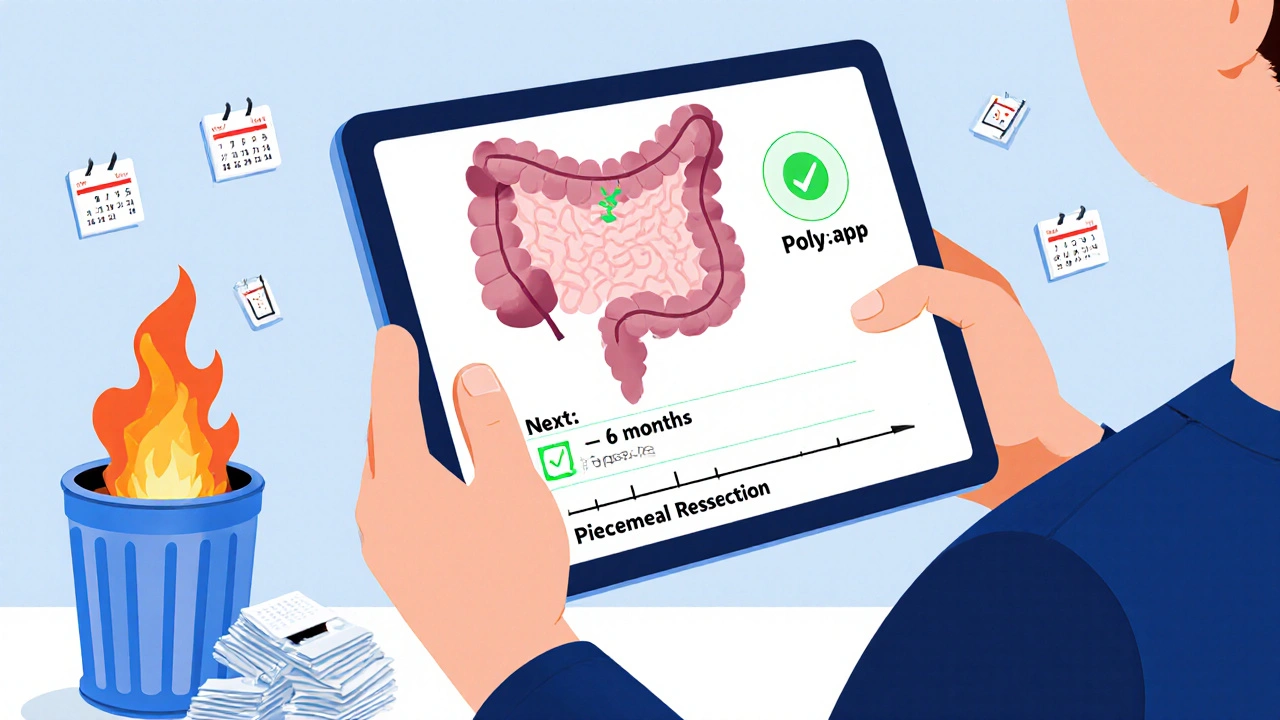
Large Polyps and Piecemeal Removal
If a polyp was bigger than 20 mm and had to be removed in pieces (called piecemeal resection), you need a follow-up much sooner. Why? Because leftover tissue can regrow.The US guidelines say: come back in 6 months. That’s a fixed rule. The European guidelines suggest a range of 3 to 6 months, but in practice, most US centers stick to 6 months. This isn’t about cancer risk - it’s about making sure every bit of the polyp was taken out.
Some hospitals do a second colonoscopy at 18 months too, especially if the initial removal was messy. But for most patients, the 6-month check is enough to confirm the area is clean.
What About Serrated Polyposis Syndrome?
This rare condition means you have a dozen or more serrated polyps throughout your colon, often with family history. It’s a red flag for high cancer risk.Guidelines vary: the Japanese recommend yearly colonoscopies. In the UK, they suggest every 1 to 2 years until age 75. If you’ve had two clean exams with no large polyps, some doctors will stretch it to 2 years. But if you’re still finding new polyps, don’t delay - stick to the yearly schedule.
There’s no room for guesswork here. This isn’t routine screening - it’s active cancer prevention.
Why So Many Doctors Get It Wrong
Despite clear guidelines, a 2022 survey found only 37% of gastroenterologists in the US could correctly identify all the risk categories. The biggest gap? Serrated polyps. Only 28% knew the right interval for small SSLs.At one Veterans Affairs hospital, only 18% of doctors followed the 7-10 year rule for low-risk adenomas. Most still said “come back in 5 years.” Why? Fear. Legal concerns. Lack of training. Even when doctors know the rules, they don’t always trust them.
Patients get confused too. Primary care providers often say, “You had polyps - you need another colonoscopy in 3 years.” That’s not always true. If you had two small adenomas, you might not need one for 10 years.
That’s why tools like Polyp.app - developed by Massachusetts General Hospital - are helping. It’s a free app that asks for your polyp details and spits out the right interval. Over 12,000 clinicians use it. If your doctor doesn’t use one, ask them to check it.
What If You’re Over 75?
Age matters. The guidelines assume you’re healthy enough to benefit from early detection. If you’re over 75, or have serious health issues, the risk of colonoscopy complications rises. At that point, the benefit of screening drops.Most experts agree: if you’ve had a clean colonoscopy in the last 10 years and no symptoms, you probably don’t need another one after 75. But if you’re 72 and just had a large adenoma, go ahead and schedule your 3-year follow-up. The goal is to prevent cancer while avoiding unnecessary risk.
What About New Tests Like Stool Kits?
Fecal immunochemical tests (FIT) and DNA stool tests (like Cologuard) are great for initial screening. But if you’ve had polyps removed, you still need a colonoscopy for follow-up. Stool tests can’t see polyps - they only detect blood or DNA changes. They’re not a substitute for surveillance.Don’t let a positive stool test replace your scheduled colonoscopy. Use it as a reminder to keep your endoscopic appointments on track.
How to Make Sure You Get the Right Interval
After your colonoscopy, ask for a written summary. It should include:- Number of polyps
- Size of each (in millimeters)
- Location
- Histology (adenoma, serrated, hyperplastic)
- How they were removed (snare, hot biopsy, piecemeal)
- Quality of bowel prep
Keep this document. Give it to your primary care doctor. Don’t rely on memory or a vague note like “polyps removed - follow-up in 5 years.”
Set a reminder in your phone or calendar. Don’t wait for your doctor to call. Most clinics don’t track follow-up intervals automatically. You have to be your own advocate.
What If You’re Still Confused?
If your doctor gives you an interval that doesn’t match what you’ve read - ask why. Show them your notes. Ask if they used the 2020 USMSTF guidelines. Most will appreciate the engagement.If you’re still unsure, ask for a referral to a gastroenterologist who specializes in colorectal cancer prevention. They’re trained to handle complex cases and know the latest evidence.
Remember: the goal isn’t to get colonoscopies as often as possible. It’s to get them at the right time - early enough to prevent cancer, but not so often that you risk complications or burnout.
With the right timing, you can avoid colon cancer without living in fear of the next scope.
How soon should I get my next colonoscopy after having one small adenoma removed?
If you had just one adenoma smaller than 10 mm and no other high-risk features, you should wait 7 to 10 years. This is based on 2020 guidelines that show cancer risk is nearly the same as someone with a normal colonoscopy. Many doctors still say 5 years out of habit, but the evidence supports waiting longer.
Do serrated polyps require different follow-up than regular adenomas?
Yes. Sessile serrated lesions (SSLs) follow different rules. One or two SSLs under 10 mm mean a 5-10 year interval. Three to four require a 3-5 year follow-up. Five or more means you need another colonoscopy in 3 years. SSLs are harder to detect and can turn into cancer faster, so timing matters more.
What if my polyp was removed in pieces?
If a polyp larger than 20 mm was removed in pieces, you need a follow-up colonoscopy in 6 months. This checks for any leftover tissue that could regrow. Even if the pathology report says it was fully removed, the 6-month scan confirms the area is clean.
Can I skip my next colonoscopy if I feel fine?
No. Colon cancer often has no symptoms until it’s advanced. Even if you feel perfectly healthy, skipping your scheduled colonoscopy puts you at risk. Polyps grow slowly, but when they turn cancerous, they can spread quickly. Follow the timeline your doctor gave you based on your polyp report.
Are stool tests enough for follow-up after polyps?
No. Stool tests like FIT or Cologuard are for initial screening in people with no history of polyps. Once you’ve had polyps removed, you need a colonoscopy for surveillance. Stool tests can’t see polyps - only detect blood or DNA changes. They’re not precise enough to replace direct visualization.
Why do some doctors say 5 years when the guidelines say 7-10?
Many doctors learned the old 5-year rule and haven’t updated their practice. Some worry about legal risk if they wait longer. Others don’t know the latest guidelines. A 2022 study found only 37% of gastroenterologists could correctly identify all risk categories. Always ask for the reasoning behind your interval - and if needed, ask for a second opinion.
Should I get a colonoscopy every 3 years if I have a family history of colon cancer?
Family history changes your risk, but it doesn’t override your polyp findings. If you had low-risk polyps and a family history, your doctor might still recommend 7-10 years. But if you had high-risk polyps, the 3-year rule applies regardless of family history. Always combine your personal findings with your family history when deciding your interval.






Comments(11)